“But I did not get any feedback on that rotation…” — Capturing feedback with a Field Note a day
Aug 7th, 2012 by Lisa Jeans
By Theresa van der Goes
But I did not get any feedback on that rotation…
Have you, as a preceptor, ever overheard a resident say this in an unguarded moment? I’m sure all of us remember those moments from our own experience as a resident, oh those long years ago.
The giving and receiving of feedback is often one of those moments that in a busy clinical setting can just flit over one’s head… and on we go to the next patient. And so many important clinical pearls can be lost along with a multitude of little learning opportunities.
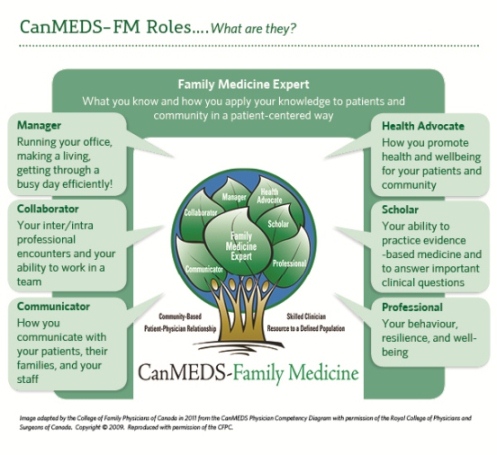
The move to Competency Based Assessment gives special emphasis to work place based assessments – taking a look at the activity of your Resident in the real live setting of an office, hospital ward, home visit or care facility. There is a new emphasis on formative assessment – all those little course corrections that are the opportunities for giving good quality feedback.
And who has time to sit and watch their resident with a patient for 15 minutes and then spend more time reviewing what you have observed? Surely, you groan, there is a faster way to just jot down a brief moment of feedback that the resident can take away to ponder later… Even better — why not have the resident jot it down, and I will just tick a box or two and sign!
Well… good news!!!
Field Notes are just exactly this: simple, fast, useful!
As of July 2012 the new cohort of Family Practice Residents will be asked to initiate the capture of that great feedback that you have been giving all along – those moments where you give relevant, specific and constructive direction … “be sure to evert the skin edges gently but fully as you place each suture – this will produce a much better scar” … “good organized knee exam – you found that meniscal tear”… or “fill in the WCB form in with the patient there – not at the end of your day! ”
And how many examples could all of us come up with in a day? One Field Note per day… let’s say 200 plus clinic days per year?!!
Good thing that the Residents are going to be keeping these little pearls, and organizing them by the Domains of Clinical Care for review by their Site Director every 4 months. They also may just share some with you, if they wish, to refresh your memory as you fill in that In Training Assessment (Web Eval) Report. You may also initiate a Field Note on your resident for any activity, especially when you observe them with your patients!
For more information see the new Field Note Guide and examples!
Related Reading
Donoff, MG. Field notes: Assisting achievement and documenting competence. CFP [Teaching Moment]. Vol 55: December 2009, 1260-126.
Dr. Theresa van der Goes is Lead Faculty for Assessment and Evaluation. She is also Site Faculty for “A & E” at the Nanaimo Site of the UBC Family Practice Residency Program.