Do you hate having your blood drawn for your lab tests? Could there be a non-invasive way to obtain your lab results? Perhaps, sweat samples could be used to measure our health status instead.
Sweating is a naturally occurring process, whether it is from exercising or getting nervous on a test. Although sweat can be perceived as wet and smelly, sweat contains various types of biomarkers, such as the stress hormone, cortisol. Since excessive stress can contribute to various health problems, such as high blood pressure, could we use cortisol in our sweats to monitor our stress levels in real-time?
Molecular structure of cortisol. Licensed under the Creative Commons Attribution-Share Alike 3.0 Unported. Cortisol.png
In a recent study, Sekar et al. has developed a wearable electrochemical sensor that can measure cortisol in sweat. The researchers has integrated iron (III) oxide (Fe2O3) in conductive carbon yarn (CCY) to make a semiconductive platform. After that, the platform is coated with antibodies (anti-Cmab) in an electrochemical apparatus, which would make the sensor specific to cortisol. The final product would then become a Fe2O3/CCY immunosensor. The purpose of the study is to see if they can use CCY as a suitable platform for biosensors when monitoring sweats.

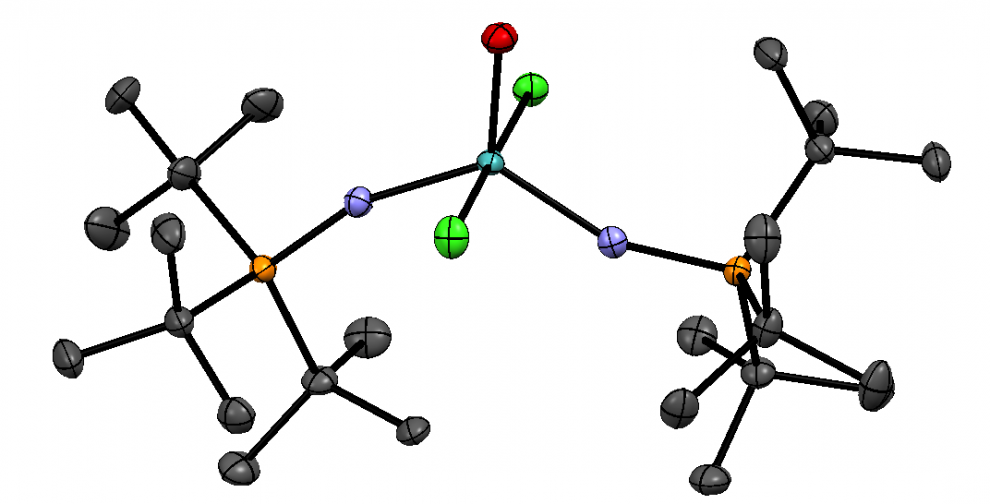
Adapted from Figure 1b in the Sekar et al (2019) paper. The black rectangle is the CCY with iron (III) oxide (orange spots). The green cylinder is the electrochemical apparatus. Licensed under a Creative Commons Attribution 4.0 International License
The researchers were able to test the sensor’s detection ability with different concentrations of cortisol. According to Figure 8b below, the line graph shows a linear relationship between the electrical current response from the Fe2O3/CCY immunosensor and the logarithm of cortisol concentration.
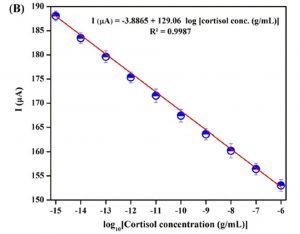
Adapted from Figure 8b in the Sekar et al (2019) paper. Each data point with error bar is the result from three successive experiments. Licensed under a Creative Commons Attribution 4.0 International License
The researchers also tested the sensor with real sweat samples from participants after performing cardio exercise. In the bar graph below, the error bars in the pink bar gives the RSD or relative standard deviation of 3.403%, 3.874%, and 4.064% from sweat sample 1, 2, and 3 respectively. These RSDs show small variations in averaged results from three successive experiments when testing with the Fe2O3/CCY immunosensor. According to the paper, the bar graph below shows a correlation between the two methods: the CLIA (chemiluminescence immunoassay) and their Fe2O3/CCY immunosensor. As a results, using CCY may be a possible choice for designing a biosensor that monitors cortisol in sweats.
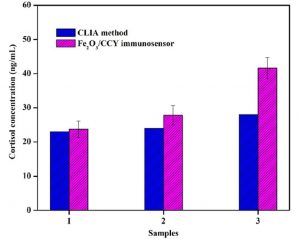
Adapted from Figure 11 in the Sekar et al (2019) paper. Each pink bar with error bar is the result from three successive experiments. Licensed under a Creative Commons Attribution 4.0 International License
In addition, there are other similar studies that focus on wearable sweat sensors, such that they can transmit data to your phone, and diagnose cystic fibrosis. Therefore, sweat sensors are potential non-invasive diagnostic tools, which may lessen the burden on more invasive blood samples to measure our health status.
References
Stress and Heart Health. https://www.heart.org/en/healthy-living/healthy-lifestyle/stress-management/stress-and-heart-health (accessed Mar 26, 2019).
Sekar, M.; Pandiaraj, M.; Bhansali, S.; Ponpandian, N.; Viswanathan, C. Carbon fiber based electrochemical sensor for sweat cortisol measurement. Scientific Reports 2019, 9, 1-14. https://doi.org/10.1038/s41598-018-37243-w.
Stephanie, Relative Standard Deviation: Definition & Formula. https://www.statisticshowto.datasciencecentral.com/relative-standard-deviation/ (accessed Mar 26, 2019).
Geddes, L. Wearable sweat sensor paves way for real-time analysis of body chemistry. http://www.nature.com/news/wearable-sweat-sensor-paves-way-for-real-time-analysis-of-body-chemistry-1.19254 (accessed Mar 26, 2019).
Dusheck, J. Wearable sweat sensor can diagnose cystic fibrosis, study finds. http://med.stanford.edu/news/all-news/2017/04/wearable-sweat-sensor-can-diagnose-cystic-fibrosis.html (accessed Mar 26, 2019).