NOTE: due to limitations in WordPress’ ability to display images with high resolution in larger sizes, if you wish to more closely examine a figure, e.g. text in graphs, please right click the figure of interest and click “Open image in new tab”.
The most common psychiatric conditions are anxiety disorders and depressive disorders, with this being especially true for university students. The two medications designed to treat these two disorders are benzodiazepines (BDZ) and antidepressants (AD) for anxiety and depression respectively. However, in addition to depression, almost all antidepressants treat anxiety and many other psychiatric conditions effectively. In the recent years, there has been a shift from doctors prescribing BDZ to AD. If antidepressants do everything that benzodiazepines do, plus more, why are benzodiazepines still prescribed at all?
First, let’s see how these drugs work. Benzodiazepines work by increasing the action of GABA, a neurotransmitter (chemical in the nervous system) that helps the brain calm down. There are many types of antidepressants, including tricyclic antidepressants (TCA; now less commonly prescribed) and reuptake inhibitors (“modern antidepressants”), which generally work by increasing levels of serotonin in the brain, a neurotransmitter that helps regulate mood, leading to enhanced mood. Figure 1 shows some BDZ and AD used in the review this article discusses.
Figure 1: Left to right: alaprazomlam, a benzodiazepine; imipramine, a tricyclic antidepressant; venlafaxine, a selective serotonin-norepinephrine reuptake inhibitor.
For those interested, the following videos illustrate detailed mechanisms of how BDZ and AD work respectively.
To see if evidence truly supports the shift towards AD from BDZ, researchers reviewed 22 studies comparing BDZ to AD in treating anxiety disorders. To keep variables constant, they compared only results from studies comparing the use of BDZ and TCA to treat panic disorder (a specific type of anxiety disorder), while analyzing the other studies individually. There were 11 such results, and those for which data was provided are summarized in Figure 2.
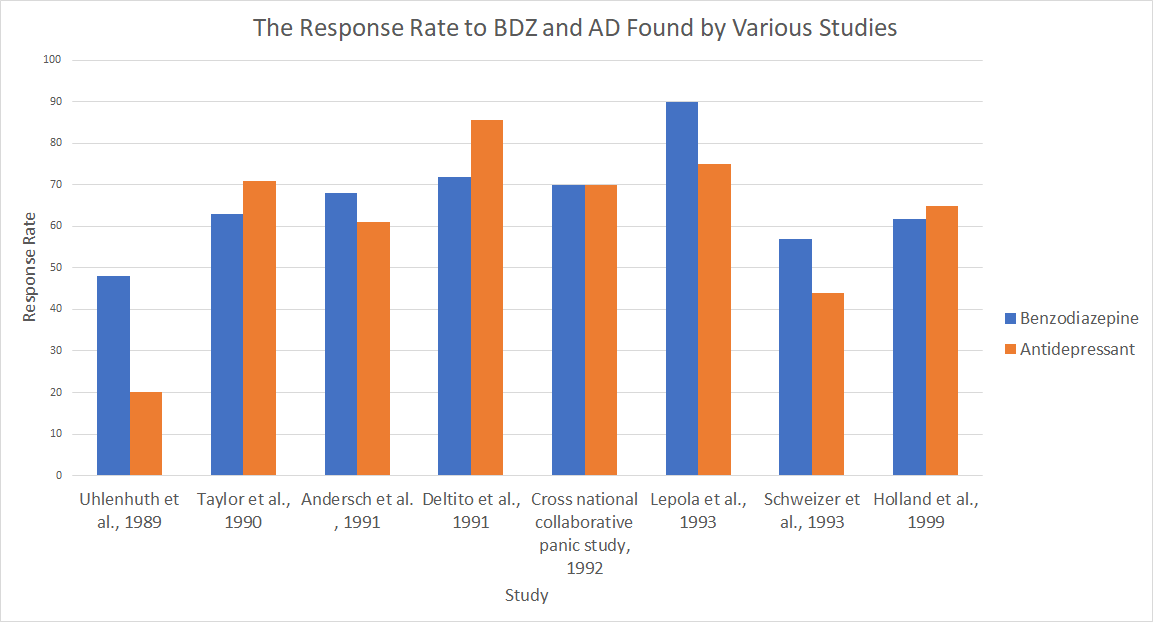
Figure 2: Response rates to BDZ and AD found by various studies. Data complied by Offidani et al.
The researchers did not find consistent statistically significant results which suggested that AD treat panic disorder more effectively than BDZ. However, in addition, they also compared the adverse events (unpleasant effects caused by medication) of BDZ and AD. Although the number of studies supplying this information was small, they consistently found that adverse events were less frequently reported for BDZ than for AD (Figure 3), and statistical analysis revealed a significant difference.
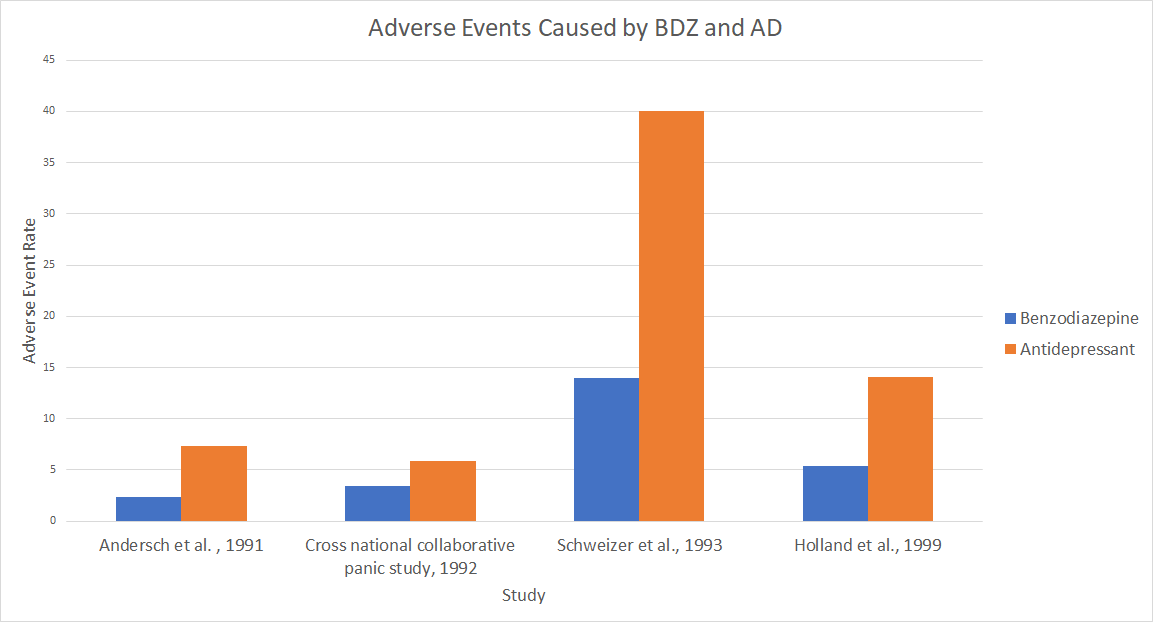
Figure 3: Adverse events caused by BDZ and AD. Data complied by Offidani et al.
Furthermore, the researchers also compared the dropout rates for the studies (which all 11 studies reported). This is the percentage of participants who, for one reason or another, chose to discontinue participation in the study. While this does not necessarily indicate that the medication is not working properly or has adverse effects, the researchers did find that BDZ dropout rates were significantly lower than those of AD (Figure 4).
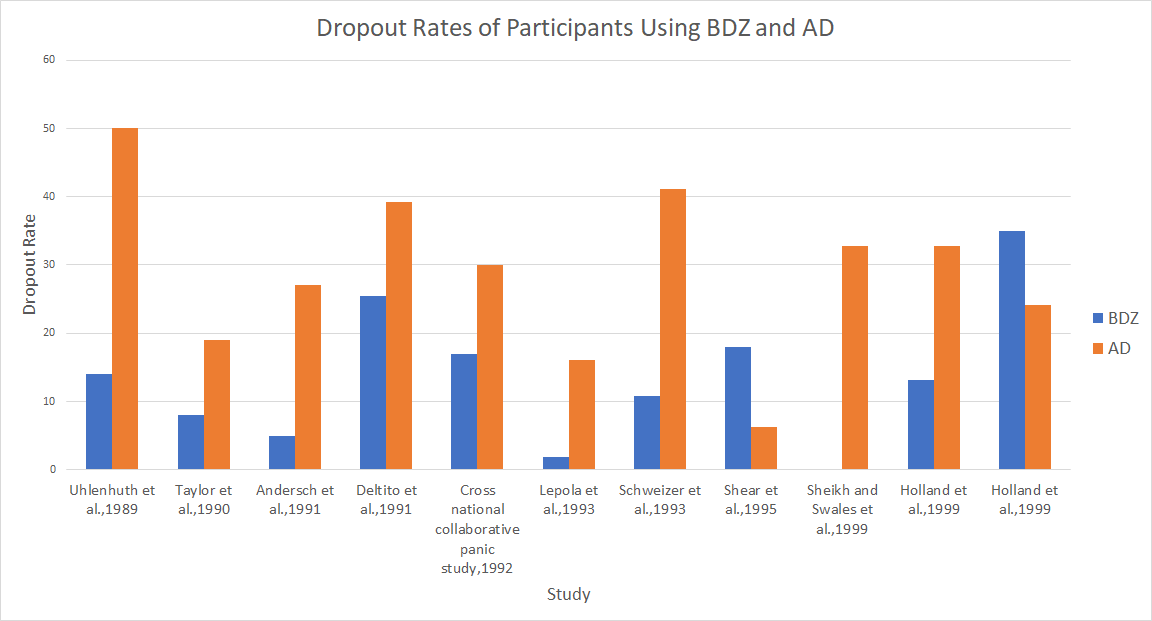
Figure 4: Dropout rates of participants using BDZ and AD. Data complied by Offidani et al.
There were only 3 studies comparing modern antidepressants to BDZ. After analyzing the data, the researchers found no significant difference in response rate between the two groups, but they found similar results for adverse events and dropout rates.
While antidepressants are undoubtedly effective at treating both depression and anxiety, there is little evidence that they treat anxiety better than benzodiazepines. That being said, benzodiazepines seem to have fewer unpleasant side effects, and therefore should still have their place in modern day medicine if anxiety alone is the issue.
-Cliff Ng
References
Schacter, D. L.; Gilbert, D. T.; Nock, M.; Wegner, D. M. Psychology, 3rd ed.; Worth Publishers, Macmillan Learning: New York, NY, 2014.
Offidani, E.; Guidi, J.; Tomba, E.; Fava, G. A. Psychotherapy and Psychosomatics 2013, 82(6), 355–362.
Offidani, E.; Guidi, J.; Tomba, E.; Fava, G. A. Supplementary Material for: Efficacy and Tolerability of Benzodiazepines versus Antidepressants in Anxiety Disorders: A Systematic Review and Meta-Analysis, 2013.
Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, 2014.
Adverse Events, Near Misses, and Errors https://psnet.ahrq.gov/primers/primer/34/adverse-events-near-misses-and-errors (accessed Feb 24, 2018).
