Source: http://bit.ly/RU3wav
A new class of polymers resistant to bacterial attachment discovered by a team of scientists at The University of Nottingham could lead to reduction in medical device failures and hospital infections.
Source: http://nbcnews.to/XzNYOh
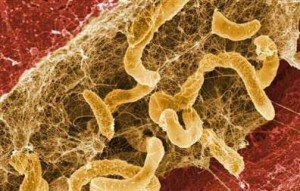
Bacteria form communities, called biofilms, on many commonly used medical devices such as urinary and venous catheters. Because biofilms are formed by a very large number of bacteria, they are resistant to bodies’ immune defenses and antibiotics. This can lead to systemic infections or device failures (devices like catheters, heart valves and prosthetic joints).
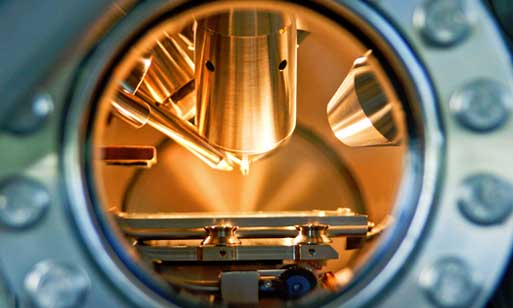
Researchers from the University of Nottingham have found that when the novel material, made of new class of polymers, was applied to the surface of medical device, it repelled bacteria.
Source: http://bit.ly/QCI5Oj
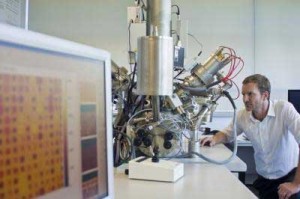
The study was lead by Dr. Morgan Alexander and Dr. Martyn Davies in the School of Pharmacy together with Dr. Paul Williams in the School of Molecular Medical Sciences. The researchers believed there were new materials that could resist bacteria, but they had to find them. They needed to screen thousands of different chemistries and test their reaction to bacteria. This was not possible using conventional methods and so they were helped by experts from the Massachusetts Institute of Technology (MIT), who developed a technology to screen hundreds of material simultaneously, looking for new structure-property relationship. This approach led to identification of novel materials which were resistant to bacterial attachment and to biofilm formation.
The new materials work by preventing infection at the earliest possible stage, when the bacteria first attempt to attach themselves to the device. This means that biofilm formation is stopped. In the laboratory setting, scientists were able to reduce the numbers of bacteria by up to 96.7% when compared with a silver-containing catheter that is available commercially. Moreover, the polymers were effective at resisting bacterial attachment in a mouse implant infection model.
Infections caused by biofilms on the surface of implants are resistant to body’s natural defenses and they often cannot be treated with conventional antibiotics. By using the new polymers, bacterial attachment would be inhibited, and the body’s own immune system would be able kill the bacteria before they would have time to generate biofilms.
To hear about this exciting discovery from the scientists themselves, watch the video below:

Source: http://bit.ly/W4vkJ8
The research has been published in August 2012 in the journal Nature Biotechnology.
Submitted by: Nesim Lichy








