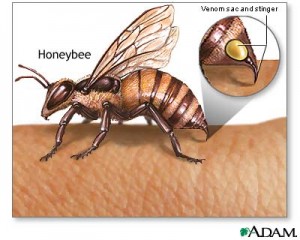
Most people that have been stung by a bee would agree that it is a very painful and uncomfortable experience that they would not want to experience again. The pain takes days to go away, and the scar that a bee sting leaves may last weeks. Now though, it looks like a bee sting may not be as bad as it seems. Researchers at the Washington University School of medicine have found that a chemical found in the venom of a bee sting can destroy the human immunodeficiency virus (HIV). What is extremely important is the fact that even though the chemical can kill the HIV virus, regular cells are immune to this chemical and are not affected by it in any way.
Researchers believe that their findings will help them develop a vaginal gel that may help prevent the spreading of the HIV virus and be used for therapy. Although they don’t think that the gel may cure the disease completely, it may be used as a preventative measure in areas where HIV is particularly common. The active chemical that researchers believe is causing the observed effects is called melittin. This chemical works by poking holes in the nuclear envelope of the virus, causing large amounts of damage that cannot be easily repaired.
To obtain their findings, researchers loaded melittin into nanoparticles and administered them to patients. These kinds of particles have been found to very effectively treat tumors, so the scientists decided to test them to see if they would be affective in treating other types of diseases. The researchers saw that when the nanoparticles came into contact with HIV infected cells they were destroyed, while the nanoparticles simply “bounced off” the normal cells, which are much larger in size.
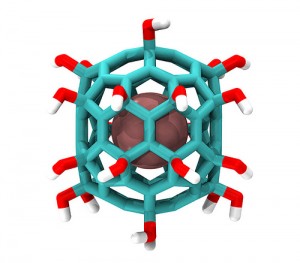
Nanoparticle incapsulating a chemical in the middle. This is the kind of mechanism the researchers used. Image from flicker user IBM Research
This is a major breakthrough in the world of science and medicine because HIV has been very hard to treat and prevent in the past. Also, HIV is a relatively common disease and many people suffer from it. It is approximated that about 36.1 million people around the world currently suffer from HIV. Furthermore, 21% of those that are infected in North America don’t even know that they are carriers of the deadly virus. Also, since the melittin loaded nanoparticles are so versatile, the researchers believe that this discovery could lead to the development of treatments for patients suffering from Hepatitis B and C.
Below is a short news report on this groundbreaking discovery:

So the next time you get stung by a bee and are panicking, calm down and just remember that the venom that the bee just injected you with is being used right now to potentially save millions of lives around the world.
Gagandeep Gill