One of the biggest concerns that has been on Canadians’ minds is the legalization of cannabis, also known as marijuana or pot. Among those who urged the legalization of marijuana, there are people who are desperate for convenient accessibility of the drug as medical pain-killers, as well as others who just need it to relieve their tired souls of this stringent world. Even though marijuana is currently only legal to prescribed patients, there is no stopping to non-patients who wish to have a joint legally. So, people wonder what difference will it make between partial and complete legalization of cannabis? How is it necessary for complete legalization of cannabis? Who does it really benefits? In order to answer these questions, it is important that we first understand how cannabis affects its users, beneficially and detrimentally.
Cannabis is a herb that has played a role in pretty much any civilizations in the past. Throughout the globe, cannabis have been used as medicines, food, and clothing. However, using cannabis became controversial in the late 1800’s and early 1900’s, for it’s recreational purposes. It became illegalized throughout the world, and is only slowly, carefully resurfacing today. The plant is most concerned for its effects on humans psychologically and physically.
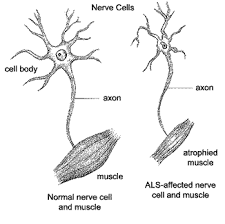
There is a reason why the federal government banned marijuana usage on the street. Such level of accessibility easily invites several groups of high-risked drug users: young teenage users, heavy daily users, and psychiatric patients. Psychologically, usage of cannabis means potentially diminished IQ’s, impaired memories, and higher risks of mental disorders. Cannabis can also induce physical harms to its users, affecting the respiratory, cardiovascular, and digestive systems.
However, there are parents around the globe who hold onto cannabis as the last resort to help their sick children. Today, in certain places, cannabis is used as pain-killers for children with epilepsy and seizures. Cannabis is also potential drugs for glaucoma, multiple sclerosis, AIDS, and cancer.
[Courtesy of CBC via YouTube]
It is unfair to straight-out condemned cannabis as an evil drug, but it is undeniably a dangerous one. As you benefit from its effects, cannabis is also working away, either positively or negatively, somewhere else in your body. So far, medical sciences can only suggest cannabis usage when there is very little a doctor can do to help patients of extreme conditions. Researchers have not yet accumulated enough studies and data to justify the usage and dosage of cannabis drugs. This article aims not to judge cannabis usage. Whether Canada chooses to support cannabis usage or not, everyone will continue to have their freedom in choosing to use, or not use, the herb. If you are interested in further topics related to drugs and addictions, here is a video about the Rat Park experiment for you to watch.
[Courtesy of MinuteVideos via YouTube]
by Esther Lo
Comments:
Can we predict the future? – Sainan Liu
Effects of Sleep Deprivation – Katherine Song
Work-life Balance – Luxi Xu