Salmonella: in Frozen Raw Tuna?
Q: What’s the big problem here with Salmonella?
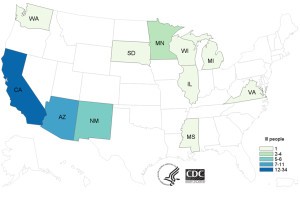
A: A Salmonella seafood outbreak that hit United States has caused 62 sick across 11 states as of July 20, 2015. US CDC reported that there were 11 cases of hospitalization and no case of deaths. 97% of the infected population recalled the consumption of sushi with raw tuna a week before becoming ill. Results from laboratory and epidemiological investigations indicated that these people were likely infected with Salmonella Paratyphi B variant L(+) tartrate(+). Raw tuna processed in Indonesia by Osamu Corporation were confirmed responsible for 18 cases in California and some cases of infections in Minnesota.
As a result, on July 21, 2015 Osamu Corporation called for a voluntary recall of two categories of items, frozen tuna and yellowfin tuna, processed in their Indonesian plant.
Q: Isn’t Salmonella usually found in eggs and poultry?
A: As known to the general population, Salmonella is often associated with foodborne illness due to its growth in poultry and egg products, as well as produce and complex foods. An interesting fact is that Salmonella is also a common pathogen found in seafood. Together with Shigella, these two pathogens constitute up to 10% of the reported foodborne illnesses in United States. Fish, shrimp, oysters and clam are food vehicles most often associated with seafood outbreaks.
Want to know more? Here is a relevant video about Salmonella in seafood (published 3 years ago):
Q: “Who” is Salmonella? Where is it from? How is it identified?
A: Salmonella is a gram negative, rod shape, facultative anaerobic, non lactose fermenting bacillus with as much as 2500 serotypes identified. Transmission routes can include food-borne and water-borne, person to person and contact with animals. According to US FDA, Salmonella can be found in seafood that is intended for minimal processing and cooking.
The source of this contamination can be traced back to the acquisition of the bacteria in polluted waters. Therefore to prevent outbreaks, current measures are carried out in harvesting waters before the final harvest. Another route of contamination can be traced to the processing and storage of the seafood.
Laboratory test of stool samples from infected patients are used for diagnosis of salmonellosis. Further tests are required to discover the subtype of Salmonella responsible for the illness.
Q: Yikes! What are the symptoms of salmonellosis?
A: Salmonellosis, an infection caused by Salmonella, can cause acute gastroenteritis, accompanied by symptoms such as diarrhea, fever, and abdominal cramps from 6 to 72 hours. Headaches, nausea and vomiting in individuals may also be visible. However these symptoms usually disappear in 4 to 7 days, when many people recover. During this period, large volume of liquid is required to replace lost fluid from diarrhea. Severe manifestations include enteric fever, urinary tract infections, bacteremia and severe focal infections. Up to 10% of patients with typhoid fever can develop serious complications.
In the circumstance of bacteremia, Salmonella can spread from intestines to blood eventually causing severe illnesses leading to death. Antibiotics may be applied to cure the disease, however antibiotic resistance is a perplex issue. Chronic pain in joints, urination pain and irritation of eyes can be some long term complications. In severe cases, chronic arthritis is observed in these patients.
Q: Who is more likely to be infected? Are there any patterns that can be observed?
A: Within the infected population, pregnant women, immuno-compromised individuals, young children (<5) and seniors (>65) are most likely at risk for developing severe disease. Consequently these individuals are advised to avoid consumption of raw finfish and shellfish. Patterns have been recorded regarding age and season: infants and elderly are on top of the list for being most vulnerable to salmonellosis; those infected individuals who consume contaminated food during the summer and early fall seasons are likely to contribute to the infection numbers.
Q: What about… specifically Salmonella Paratyphi B variant L(+) tartrate(+)?
A: Salmonella Paratyphi B variant L(+) tartrate(+) (formerly Salmonella Java) belongs to the subspecies of Salmonella enterica and is known to cause non-typhoid salmonellosis. In contrast, Salmonella Paratyphi B variant L(+) tartrate(-) causes paratyphoid fever.
Q: How should we “wrestle” with the pathogen especially in seafood?
A: Besides usual ways of avoiding foodborne illnesses, effective methods of preventing foodborne illness in specifically seafood, as suggested by US FDA, include:
- Washing hands, utensils and cooking surfaces
- Cooking seafood for 15 seconds at minimum of 145oF
- Avoid cross contamination by separating raw and cooked seafood
- Storing seafood below 40oF in the refrigerator or below 0oF in the freezer
And finally… Questions for you!
- What is a possible reason for Salmonella to be able to grow in frozen raw tuna?
- What are some possibilities that the infection cases can occur over 11 states (possible routes)?
Salmonella in raw tuna articles:
http://bigmedicine.ca/wordpress/tag/salmonella-paratyphi-b-variant-l-tartrate/#sthash.VN7LcdMj.dpbs
FYI… Check it out! (References:)
Epidemiology of Seafood-associated infections in United States:
http://cmr.asm.org/content/23/2/399.full
Facts on Seafood safety:
http://seafoodhealthfacts.org/seafood_safety/practitioners/microbes.php
Salmonella Q&A:
WHO document on Typhoid Fever:
http://www.who.int/rpc/TFGuideWHO.pdf
WHO document on Non-typhoid fever:
http://www.who.int/mediacentre/factsheets/fs139/en/
Government of Canada guidelines:
Paratyphoid fever:
http://www.health.alberta.ca/documents/Guidelines-Paratyphoid-Fever-2014.pdf
Youtube video on this case:

csontani 4:37 pm on November 21, 2015 Permalink |
First of all, I really like how you format your blog! It’s definitely easy to read since the questions really help the readers to stay focused on the topic. Anyways, I think that most people just assumed that they can only be infected by Salmonella from eating raw eggs and poultry (in this case, there should be another way to inform people that it’s not limited to those sources). I remember getting infected with Salmonella couple of years ago from eating raw salmon, which I thought isn’t possible. But then I’m from Indonesia and I’m definitely not surprised that many people were infected by pathogenic bacteria from food. But I think that possible ways that the seafood is contaminated with Salmonella would be during the thawing process. And since they determined that all of the cases lead back to one source, I think that the main problem started from Indonesia where the tuna was imported from.
dgozali 1:42 am on November 23, 2015 Permalink |
Very interesting blog post and really great organisation of information! I think this really highlights the point that Salmonella can be associated with other types of food besides poultry and eggs. This personally scares me a little as I really love eating sushi and raw seafood. One of the reasons that Salmonella could have survived in frozen fish perhaps could be due to cross protection. If the pathogen was exposed to sublethal treatments it could develop resistance to subsequent steps in processing.
TamaraRitchie 9:54 am on November 23, 2015 Permalink |
Very nice layout. This was really easy to read and reminded the reader of key points. I think it may be possible for Salmonella to grow in the frozen tuna because freezing the sample will not kill Salmonella, it will just inhibit the growth, therefore when the tuna comes to room temperature when being served at restaurants it could cause illness and the bacteria could start to multiply. I think it is possible that the cases were so wildly spread because this company possibly distributed this product to varying states.
angel519 1:37 pm on November 24, 2015 Permalink |
As mentioned in the blog, improper handling practices during processing and store can contaminate the raw seafood with Salmonella; I think for seafood especially sashimi grade seafood, it is very crucial to have proper handling practices and clean production area to avoid contamination. Because Salmonella can survive the freezing storage temperature, once the seafood is defrosted, the pathogen will be able to start replicating and grow.
RainShen 11:23 pm on November 24, 2015 Permalink |
It is interesting that the frozen tuna was processed in Indonesia, which is such a far place in Asia. I’m not sure how the company transported the tuna to US, by ship or by air. If the frozen tuna transported by sea then it was possible the products underwent temperature abuse during the long distance transportation. Even if the tuna transported by air, the products may thaw a little during the transferring between different vehicles, e.g. truck and airplane. If Salmonella was in the tuna in the first place then it’s very difficult to eliminate the pathogens after, since Salmonella can survive under very low temperature. I agree that improper handling can be one of the main causes of the contamination as well. Foods like sashimi is very hard to cook for 15 seconds at minimum of 145F, which may loss the texture and raw taste.
KristinaRichmond 8:59 pm on November 27, 2015 Permalink |
Nice article! I agree that there are many points at which the fish could have become contaminated- poor storage temperature, thawing, or cross contamination all could have played a role in this outbreak. I always assumed that sushi fish would be sourced locally and a lot fresher. This goes to show that you really need to be a conscious consumer, and take the time to think about where the products you’re eating are coming from. However, I think sushi is a higher risk food and all this could have happened with local fish too, so it’s probably important for vulnerable individuals to avoid eating it.
Stephanie Chen 6:13 pm on December 1, 2015 Permalink |
Great organization of points! Importing the processed tuna from an overseas plant creates many more opportunities for contamination to occur. As the product is being transferred from place to place, and then furthered processed for consumption, multiple points could have allowed thawing and growth of Salmonella. According to the FDA Food Code (http://www.fda.gov/downloads/Food/GuidanceRegulation/RetailFoodProtection/FoodCode/UCM374510.pdf), certain temperatures and times for freezing are designated to kill parasitic worms. But this of course does not guarantee that raw fish products can become pathogen free. I agree that freezing only slows or inhibits the growth of Salmonella. However, it is truly a challenge for heat treatment of these foods that are intended to be eaten raw. Therefore, sanitary handling practices are crucial in decreasing risk of contamination.
cheryl lau 3:14 pm on December 4, 2015 Permalink |
This is an interesting article as Salmonella outbreaks are not typically associated with seafood. As stated in the article, the contaminated tuna was processed in Indonesia. Perhaps the cold temperatures that the products were subjected too were not cold enough to kill the bacteria and actually activated the stress proteins that made them survive other subsequent sub-lethal stresses. If the company was distributing the fish to the 11 states, perhaps their storage facilities or the mode of transport was contaminated and it could have affected all the shipments. Personally, I feel like there is always a risk when eating raw or partially cooked foods, but it would be a shame to give them up because of a fear of contamination. As long as restaurants or processors follow the proper handling procedures, consumers can feel safe enjoying these delicacies.
meggyli 11:48 pm on December 4, 2015 Permalink |
This is a really interesting layout for a blog with the Q&A. I don’t think I’ve seen anyone else do their blog this way! The Q&A definitely makes the blog easier to follow and highlights the important points. Again, it’s an article on a foodborne illness in which the pathogen involved is not commonly associated with the food. This article highlights the risks and dangers of operating a plant for raw and spoil-prone food, and in this case, tuna. Getting them overseas may be the cheaper option, but I feel that the risks associated with the long-distance travel and storage are not worth the money saved. Personally I would prefer eating locally farmed or wild seafood.
yichen25 1:02 am on December 11, 2015 Permalink |
I really enjoyed reading your blog post as the flow is well thought over. As for the questions you mentioned, I personally think that there is a possibility of the activation of stress response which enabled Salmonella to survive in extreme conditions, as learnt in FNH 413. Also, the stress response activated in Salmonella can also be applied in the survival in the host’s environment which further enhance their virulence. Therefore, it is vital to only consume raw seafood if it is certified to be safe for consumption or always cook the seafood to ensure the elimination of the seafood. I personally am a Sashimi lover and I guess one of the ways to avoid consuming contaminated seafood will be to only eat in a restaurant which is well reputable for the preparation of raw seafood.
Carissa Li 1:56 am on December 14, 2015 Permalink |
Your article is among all the simplest to read since they all start with a question and your answers are very detailed! It is very shocking to know that even frozen tuna can be contaminated by salmonella. Firstly is because it is rare to see samonella appear in seafood and secondly, we never learned that salmonella is tolerant to low temperature so this article really opened my mind! Eating raw food always has an increased risk of getting foodborne illnesses so getting the regulation straight and letting people know how to properly handle and prepare raw food is an important step to prevent any foodborne illness outbreak.
CindyDai 12:07 am on December 15, 2015 Permalink |
I really like your Q & A formatting. It really makes the blog more interesting and attractive to the general public. Public education on food safety practices is the most efficient way to prevent cross-contamination at the household level. It is also very interesting to know that Salmonella can survive cold treatment, such as freezing and refrigeration, and be present on raw seafood products. This indicates the importance of controlling initial contamination at the primary food production site. If we want to keep enjoying sashimi, microbiological quality control tests at the farm level are definitely necessary.
JorgeMadrigalPons 11:45 am on December 15, 2015 Permalink |
Salmonella is a very flexible organism and it can be a problem in many food products. When talking about seafood, preventing contamination may be difficult. Since seafood is often eaten raw, killing salmonella by cooking or high temperatures is not possible. Washing the tuna before preparing the dish might be a good preventive method.
CandiceZheng 2:47 pm on December 15, 2015 Permalink |
Salmonella again?!! It is such a nasty microorganism that would exist EVERYWHERE in our food system. I really appreciate the organization of your post: not only did you use the Q&A format, which makes the blog post very clear and simple to use, but the logic flow is clear and easy to follow. Besides, I like the practical advise you gave at the end. They are very helpful and easy to follow, and also based on scientific evidence that we learnt in class.