_supply/3
Recent Updates Page 3 Toggle Comment Threads | Keyboard Shortcuts
-
ColleenChong
-
JorgeMadrigalPons
Virus Outbreaks in Europe linked with frozen berries.
In Europe, there have been recent concerns regarding consumption of frozen berries. Unfortunately, Hepatitis A virus (HAV) and norovirus have been linked with these nutritious and tasteful produce. Authorities and food industries have struggled with large and prolonged food-borne outbreaks.
The most recent incident involving HAV and frozen berries lasted from 2013 to 2014. This outbreak began in May 2013, when Germany reported seven hepatitis A cases in travellers coming back from northern Italy. Subsequently, Italy declared the first national outbreak, and other European Union countries reported locally acquired and travel-related cases of HAV associated with the same problem, consumption of berries. From January 2013 to August 2014, 1,589 hepatitis A cases were reported linked with the frozen berry outbreak. 70 % of these cases were hospitalised for an average time of six days, and there were 2 deaths reported (Severi et al, 2015). Trace backs done by the European Food Safety Authority could not indicate a single point source of contamination (RASF, 2015). The frozen berry market in Europe is very complex, considering the produce can be distributed at different times in different countries. Although it is not fully certain, the main suspicious candidates to blame were Bulgarian blackberries and Polish redcurrants, since these were the most common ingredients in the different contaminated samples.
Regarding norovirus and frozen berries, from 20 September through 5 October 2012, the largest recorded food-borne outbreak in Germany occurred. Norovirus was spotted as the causative agent. 390 schools and childcare facilities reported nearly 11,000 cases of gastroenteritis. All affected institutions had received strawberries of one lot, which lead to the identification of frozen strawberries from China as the most likely vehicle of infection. Thanks to the timely surveillance and epidemiological outbreak investigations of the correspondent authorities that detected the case within a week, more than half of the lot was prevented from reaching the consumers (Bernard et al, 2014).
The occurrence of outbreaks associated with frozen berries has raised many concerns, especially with the growth in popularity of fruit-based products like smoothies, ice creams and yogurts. According to literature, in a period from 1998 to 2013, frozen berry contamination with norovirus caused 14,000 reported human cases in 70 outbreaks in six EU countries, namely Denmark, Finland, France, Germany, the Netherlands and Sweden (Tavoschi et al, 2015). The European Food Safety Authority highlights the risk of contamination of berries, because this food commodity often receives no or minimal processing. Contamination and cross-contamination via equipment, water (irrigation and washing) and particularly via food handlers have been identified as the main risk factors (Tavoschi et al, 2015). Also, it is known that viruses like NOV and HAV, can resist freezing treatments and remain latent in the product, which make frozen berries a perfect source of contamination. Since there have been new outbreaks this year (norovirus in Sweden and hepatitis A in Australia), European authorities recommend to be careful when consuming frozen berries. They specially suggest to boil imported frozen berries for one minute before eating, especially if the food is going to be given to vulnerable people such as nursing home residents (FSAI, 2015).

References
Severi, E., Verhoef, L., Thornton, L., Guzman-Herrador, B. R., Faber, M., Sundqvist, L., … & Tosti, M. E. (2015). Large and prolonged food-borne multistate hepatitis A outbreak in Europe associated with consumption of frozen berries, 2013 to 2014. Eurosurveillance 20, 29. Retrieved from: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=21192Tavoschi, L., Severi, E., Niskanen, T., Boelaert, F., Rizzi, V., Liebana, E., … & Coulombier, D. (2015). Food-borne diseases associated with frozen berries consumption: a historical perspective, European Union, 1983 to 2013. Euro Surveill, 20, 29.
RASFF (2015). The Rapid Alert System for Food and Feed, Annual Report 2014. European Commission – Health and Food Safety.
FFSAI. (2015). Berries – Advice to boil imported frozen berries. Food Safety Authority of Ireland. Retrieved from: https://www.fsai.ie/faqs/berries_advice_to_boil_2015.html
Bernard, H., Faber, M., Wilking, H., Haller, S., Höhle, M., Schielke, A., … & Stark, K. (2014). Large multistate outbreak of norovirus gastroenteritis associated with frozen strawberries, East Germany, 2012. Eurosurveillance, 19(8), pii-20719.
-
Jasmine Lee
Great post, Jorge! It is frightening that enteric viruses, specifically HAV and NOV, are highly resistant to many hurdles and common processing methods, e.g. freezing and desiccation. This is quite unfortunate and worrisome as frozen and dried fruits are versatile ingredients and widely used in many recipes. Consumers typically depend on these preserved products as not many fresh fruits are in season and they are quite expensive during the winter. I agree that boiling may be the most feasible method for viral inactivation aside from commercial sterilization. Canned fruits, sauces and fillings may serve as an alternative and safe (assuming the absence of C. botulinum) source of nutrients for vulnerable groups. Another point to note is that these outbreaks highlight the importance of adherence to proper hygiene practices from farm to fork. Therefore, do you agree that more stringent regulations should be in place for controlling enteric viruses, especially for imported goods?
-
wen liao
This is actually a really interesting post! Usually when we think about viruses and such, we think about pandemic flus and something that is airborne. However, a large amount to GI tract related disease are largely contributed to viruses. Especially for fresh produce such as vegetables and fruits, rarely do we link them to HAV contamination and infection. Comparing to bacteria, viruses are more resistant to some environmental stresses, and they their virulence stays unchanged even after freezing or other production hurdles. I am not sure if there are some developed essays that are specific in targeting these viruses, but it should definitely considered as a big public health problem.
-
NorrisHuang
Interesting! It is scary to learn about this. I am a big fan of berry smoothie but I don’t think I am gonna boil the berries before blending them up as the texture/ taste may change, and also, the smoothie may become too watery. (using canned berries may be a good idea though) I wonder if there is another way of getting rid of the viruses in addition to boiling? If not, I guess it is the most effective to prevent the virus before harvesting the berries? and also, how is the viruses regulated in North America?
-
EmilyLi
I think this is a great story. Frozen food are processed and kept at low temperatures (at least below zero degree Celsius). With that reason, many people have the mind set that many of the microorganisms that may cause illness would not be present in the food. Like many people, I wouldn’t give a second thought about consuming my frozen fruits. I like how this instance will bring awareness that ready to eat frozen aren’t always safe for consumption either. In my opinion, consistent analysis and checking the food product for various microorganisms before the food product being release in the market would be a good solution for food companies to adopt.
-
elaine chan
Definitely an interesting post! As mentioned, it’s not common for consumers to associate frozen fruit products to an outbreak like this. As a Food Science student, I would also not give much thought as to how frozen fruits can be contaminated like this, as the processing procedures are relatively simple compared to other food products. I’m really glad that the surveillance and epidemiological outbreak investigation prevented another wave of outbreak from happening, and I feel that all food agencies across the globe can learn from this to prevent any sort of food break to occur. However, I do question the practicality of the advice provided by the European authorities of boiling the fruit product prior to consumption. Majority of the population consumes fruit in its raw form; thus, this advice seems rather impractical and difficult to adapt by consumers.
-
meggyli
Reading this post made me sad, because frozen berries are one of my favorite ingredients in a morning smoothie. 🙁 For something that is processed and stored in such a low temperature we usually don’t think about it possibly being contaminated with a pathogen. Even as a Nutrition student this is not something that would spring up in my mind when I think frozen berries. Therefore I think it is even more important for the public to be aware of such occurrences. I really enjoy the blogs on this site that highlights the outbreaks associated with uncommon foods.
-
-
dgozali
Norovirus Outbreak on Cruise Ships
It’s a month before the end of the term, stress levels are rising as deadlines draw near and we count down the days before finals start. A holiday cruise seems like a perfect way to unwind and relax during your break from school or work. This was what passengers of Star Princess thought on September 19, 2015 when they boarded their 2-week long cruise to the Hawaiian Islands. Little did they know that they were about to suffer the effects of a Norovirus outbreak. On October 4th 2015, Star Princess docked in Vancouver with a total of 61 passengers who were sickened by Norovirus and displayed symptoms of acute gastroenteritis such as abdominal pain, nausea, vomiting and diarrhea. The Virus was spread through contaminated food, water and personal contact. Earlier this year, the same cruise ship experienced another Norovirus outbreak that affected a total of 135 passengers.
The cruise ship reportedly stopped at several ports where sick passengers were taken to the hospital for further treatment. Several passengers even took a flight back from Hawaii instead of continuing the journey on the cruise. In order to prevent the further spread of the virus, several measures were implemented on the cruise ship:
- Disinfection of hand railings, door handles and elevator buttons
- Hand sanitizers were placed on several locations on the ship
- Infected passengers were isolated from the rest of the passengers
A single food source has not yet been identified for the cause of this outbreak. However, the Food and Drug Administration states that the most common sources of Norovirus include water supply on cruise ships and raw oysters, fruits and vegetables. Once the virus has infected someone, it can be easily transmitted through close contact or cross contamination. A big issue with eating contaminated food on cruise ships is that the sewage and waste produced on cruise ships is dumped 12 miles from the shore. This results in contamination of shellfish that filter-feed around the area where waste was disposed. These contaminated shellfish are then harvested and consumed by people on shore, leading to more infections or outbreaks.
Norovirus outbreaks seem to be a recurring phenomenon on cruise ships with a total of 9 outbreaks recorded in this year alone. But why is Norovirus so notorious for causing outbreaks on cruise ships? Firstly, outbreaks on cruise ships are generally reported more quickly than outbreaks on land. Cruise ships also provide an ideal condition for the spread of Norovirus as it is an enclosed environment that increases the amount of person-to-person contact within the shared living space. The common source of food and drinks also facilitates the spread of Norovirus infection. Lastly, about a third of the passengers on cruise ships are elderly people who are more susceptible to Norovirus infections, which results in a greater incidence of infection.
Due to the high occurrence of this issue on cruise ships, Centers for Disease Control (CDC) has created a surveillance and reporting system to prevent and reduce the risk of spreading gastrointestinal illnesses. CDC’s Vessel Sanitation Program monitors the magnitude and distribution of cases reported, helps to implement sanitation procedures, makes recommendations for control of the pathogen and conducts investigations to determine the causative agent. If the illness rate on board the cruise is 3% or more, an investigation is performed through 3 main steps:
1) Epidemiological investigation: Measures the size of the outbreak through questionnaires, medical records and cruise ship layout.
2) Laboratory investigation: Specimens collected from infected passengers to confirm the pathogen responsible.
3) Environmental investigation: Uses information from the epidemiological investigation and further investigations to determine the source of infection.After learning about the occurrence of Norovirus outbreaks on cruise ships, would you still consider going on a cruise? Can you think of any other ways that this issue can be prevented?
Sources:
Bert, F., Scaioli, G., Gualano, M. R., Passi, S., Specchia, M. L., Cadeddu, C.. . Siliquini, R. (2014). Norovirus outbreaks on commercial cruise ships: A systematic review and new targets for the public health agenda. Food and Environmental Virology, 6(2), 67-74.
Centers for Disease Control and Prevention. (2015). Outbreak updates for international cruise ships. Retrieved from http://www.cdc.gov/nceh/vsp/surv/gilist.htm#2015
Centers for Disease Control and Prevention. (2015). Outbreak Investigation Overview. Retrieved from http://www.cdc.gov/nceh/vsp/surv/investigationoverview.htm
Canadian Broadcasting Corporation News. (2015). Norovirus hits Star Princess, delays massive cruise ship in Vancouver. Retrieved from http://www.cbc.ca/news/canada/british-columbia/star-princess-cruise-norovirus-hawaii-vancouver-b-c-outbeak-1.3255632International Business Times. (2015). Cruise Ship Norovirus Outbreak 2015: Dozens of Star Princess Passengers Sickened By Stomach Bug. Retrieved from http://www.ibtimes.com/cruise-ship-norovirus-outbreak-2015-dozens-star-princess-passengers-sickened-stomach-2127270
-
csontani
it’s funny cause I was actually on board another Princess cruise last August around British Isle and that ship had a Norovirus as well before my sail. I think for that case it was because of the spread from 1 infected person that boarded on the ship. I agree that there are numerous outbreaks that occur in cruise ships because they’re pretty much “isolated” in one place. Cruise ships should definitely be more strict in checking the passengers’ conditions before they board the ship. From what I see so far, they only have questionnaires that they hand out to the passengers, asking if they’ve been sick for the past couple of days/weeks, and I personally think it’s not effective cause people can just easily lie about it. So they should definitely think of a better way to monitor passengers health conditions before sailing.
-
cvalencia
It is challenging to be on a cruise and find out that there is currently an outbreak going on… I can’t imagine having that constant worry in your mind that you or your family members might be the next ones to get ill. It just ruins the whole point of going on a cruise and having a peaceful vacation alone or with your loved ones. It’s also hard since there are little to no other options for other foods once you’re on the ship, but the ones that they serve on the buffet and cafes. I also think that it is devastating not only for the passengers but also for the cruise company, since they will now have a bad reputation because of these outbreaks. It’s great to know though that the CDC are providing guidelines to prevent future outbreaks.
-
Silvia Low
This is so saddening to hear. I love cruise ships but I have heard of the many onboard outbreaks they often have. My understanding of how they reduce the risk of infection/contamination is by having their employees serve all the food at the buffet instead of passengers self serving. Anyway, I donot think any one cruise company should have their reputation or brand tarnished because of this because it could also be the passengers’ fault for bringing infectious illnesses onboard and the cruise companies do specifically ask all passengers if they’re sick or experiencing any symptoms prior to boarding.
-
shinnie
I believe that the newly implimented measures to prevent the spread of the virus on cruise ships will not be as effective as perceived. In fact, it may worsen the spread of the virus if the employees are led to think that hand sanitizers alone are enough to eliminate the pathogens. If sanitizers with insufficient ethanol content are used (60-65% of normal hand sanitizers is NOT enough), norovirus will not be eliminated. Studies show that hand sanitizers are useless against norovirus because the virus is non-enveloped and protected by a capsid. Statistics from the U.S. Centers for Disease Control and Prevention in winter of 2006-2007 show that “facilities in which staff used alcohol-based sanitizers were six times more likely to have an outbreak of norovirus compared to those in which staff cleaned their hands using soap and water.” The best methods to minimize norovirus outbreaks on cruise ships include minimizing food contact or food contact surfaces with bare hands and using extremy hot water and bleach to clean dishes and stainless steel surfaces. Proper hand washing should be strongly enforced on cruise ships as studies show that they are more effective in eliminating norovirus than sanitizers due to physical foce. For me personally, I will probably go on a cruise expecting to catch some kind of stomach flu.
-
Carissa Li
I was on a cruise ship this past summer too and I can relate how quickly an infection can be spread inside an enclosed environment. In my case, one of my family members caught a flu before the trip start and within 2 days, 5 other family members got infected with the flu. How quickly that was! With norovirus, I think the rate can get even faster since everyone is consuming the same food which is only one of the several routes Norovirus can take to infect people. I know that one of the surveillance cruise ships take is once they identified anyone who’s at risk, they will send them to the hospital at the next port they arrive. It is very important to make sure we all get sanitized before walking into any restaurants on the ship so as to prevent any bacteria contaminating the food as well as prevent ourself getting infected by others.
-
teewong
I agree with this post entirely about the fact that cruise ships are more susceptible to these types of outbreaks as people are confined in a close proximity area. I was planning on booking a cruise trip this coming summer and this really made me second think my decision. I think if I were to follow through with my decision in booking a cruise trip, I would bring my own cutleries and personal towels to minimize any cross contaminations with other passengers.
I was also wondering, in the post it didn’t mention what the cruise company did to compensate the passengers that fell ill from this infection, did they compensate these passengers at all? -
MichelleLui
Cruise ship can certainly provide an environment that facilitate the spread of foodborne illnesses. Good personal hygiene and sanitation program should be followed by cruise ship workers. Passengers should be prepared and take preventative measures such as immunization and follow good hygiene practices (e.g. wash hands often).
-
YaoWang
Grocery store loyalty cards help B.C. disease detectives trace hepatitis A outbreak
Hepatitis A virus can cause Hepatitis A, which is a potentially serious form of liver disease by attacking the liver. Non-travel-related hepatitis A infection is rare in North America as the virus is usually found in developing countries with very poor sanitary conditions and hygiene practices.
It often takes a long time to recognize that a food-borne disease outbreak is underway because cases can be dispersed geographically. Taking into consideration that the incubation period of hepatitis A is usually 14 to 28 days, it can be difficult to find the source since people cannot recall with precision what they ate weeks earlier.
An example of successful investigation is the recall of hepatitis A contaminated pomegranate seeds in British Columbia in early 2012 by comparing the foods the infected people had bought in previous months. Those food purchasing histories were compiled from their crockery story loyalty cards, pomegranate seeds in a frozen fruit mix were eventually identified as the source of the infection. At a very early stage, with only six cases, the investigators were able to see that the infected people had purchased the same brand of a frozen fruit mix containing blueberries, strawberries, cherries and pomegranate seeds. The following test eventually showed that on e lot of pomegranate seeds from the supplier was contaminated with hepatitis A and a recall was ordered.

“It certainly did make it easier and it allowed us to identify, to really land on a specific product really very early in the outbreak,” Dr. Helena Swinkels of Fraser Health Authority says of the access to the patients’ purchasing history through their loyalty card data, “Loyalty cards are one tool that definitely can help investigations of food-borne outbreaks.”Although hepatitis A is rare in Canada and the few cases recorded each year generally are in people travelling in or returning from countries where the virus circulates, occasionally someone who becomes infected will transmit it to others in Canada. Therefore, it is necessary for the public to understand its transmission pathway and the prevention methods.
Transmission:
-Faecal-oral route
-Waterborne outbreaks, infrequent, usually associated with sewage-contaminated or inadequately treated water.
-Close physical contact with an infectious person, although casual contact among people does not spread the virus.Prevention:
-Improved sanitation, food safety and immunization are the most effective ways to combat hepatitis A.
-Several hepatitis A vaccines are available internationally.
http://www.streamingwell.com/how-do-you-get-hepatitis-a-video.htmlSources:
http://www.liver.ca/liver-disease/types/viral_hepatitis/Hepatitis_A.aspx
http://o.canada.com/health-2/grocery-store-loyalty-cards-help-b-c-disease-detectives-trace-hepatitis-a-outbreak
http://www.who.int/mediacentre/factsheets/fs328/en/-
CandiceZheng
Using the loyalty card is a very interesting and a new way to track the food that is responsible for the food pathogens. Although there might be some privacy concerns, the information era do help us a lot.
-
Susanna Ko
That’s really interesting. I wonder if they use credit card and debit card tracking to trace back those who purchase affected foods as well. It’s also scary that Hepatitis A is found in berry mixes, in which consumers will make smoothies and drink it raw.
-
yichen25
Wow, I never thought that grocery’s loyalty card can play such a huge role in a recall investigation. Since it is such an efficient tool to be used to track food purchase history, perhaps they can adopt this method and use it in a larger scale. For example, the Government can come up with initiative to propose a card system where consumers track their food purchase history nationwide. This can be done in collaboration with grocery stores and restaurants.
-
RainShen
This is the first time I heard that grocery store loyalty cards can help investigate the foodborne illness infection and recall. Actually this can be applied widely to even restaurants since a big portion of the foodborne illness happen in the restaurants. Since many customers would not pay attention to the food safety news or the recall announcement after they purchase the food products, they may still consume the infected foods which have been recalled. I think if a tracing back system can be built up using loyalty cards will be very useful.
-
angel519
I agree with Yichen that the Government can utilize a card system to track consumers food purchase history. If a person got sick, they can quickly identify the suspicion food product; and if an outbreak happens, this system can group all the patients food record and find out the common food product. If this card system is in use, it will speed up the foodborne illness investigation process and reduce in personnel costs.
-
DeniseZhang
I think this is very interesting. Never thought that the loyalty cards could help to trace back the purchases, as we only regard this as a method of saving money. I guess after this outbreak many people started to get a loyalty card not just for saving money but for health issues (just kidding). However, I am quite curious about those who did/do not have a loyalty card. How to trace them down then?
-
MarinaMoon
It’s really interesting to see that loyalty cards played a very important role in detecting the virus. As hepatitis A viruses can result in serious liver damage, it’s good to hear that it has been detected early in the outbreak. I also agree with Yichen with having cards that can track grocery listings and other food consumptions made by an individual. This would help the detection method a lot faster and lead to better prevention in the future. Since there are more and more pathogens that are developing in food and increased number of outbreaks around the world, these kind of implementation seem very efficient.
-
WinnieLiao
Thankfully that non-travel-related Hepatitis A is uncommon in North America, but there is definitely still a need to be aware of it! It’s interesting how loyalty cards can be helpful in an outbreak investigation! Tracing back the purchase and recalling the product can definitely helpful. It would be a helpful too if the customer signed up as a member, in addition to collecting points and benefits, the system records the products that the customer has purchased. Maybe in this way the recalls can be easier done because the personal information of the customer can quickly be found.
-
Stephanie Chen
I agree with Susanna that it is quite scary to know frozen berries may be contaminated with Hepatitis A. Many consume this type of product raw without awareness that it may even be a source of foodborne pathogens at all. This is also a very interesting way of finding the source of outbreak! By searching for a common thread among purchasing records, the time of investigation can really be shortened. Maybe because of this, customers would be more willing to put down their actual information when having to fill out forms at food retails stores as well!
-
meggyli
This is such an innovative and simple way of tracking our diet records I can’t believe no one has thought of it before! Thank you for the eye opening article. One of the largest hurdles to correctly identifying the source of a foodborne outbreak is the patients being unable to recall food they have eaten a while ago, especially for pathogens with a long incubation period. By being able to access their shopping record can no doubt prompt their memories if not recall completely. We can even make this a larger-scale project by having all sorts of supermarkets and restaurants participate, in which the consumer may have the option of recording down their purchase every time they visit. Not only will this benefit health officials and merchants, consumers can also benefit from being able to recall their favorite food from favorite places at a moment’s notice. Personal information exploitation, however, is still a concern, which should be tightly regulated if this were to happen.
-
CindyDai
I never know that grocery membership cards can be used in outbreak investigation, and it really inspires me of how creative data collection could be. As Dr. Wang said in the Big Data lecture, the way of thinking is consistently changing. How to discover potential source of data has recently become crucial in systematic problem solving. Even after data collection, the 4V of the data could also influence the final outcome. People should take more advantages of Big Data, and invent more applications of Big Data in food safety survellence and outbreak investigation.
-
dgozali
I love how creative this method is used in investigating an outbreak! Its not only simple but also very accurate way of obtaining the necessary information. Just as meggyli mentioned, people might not be able to remember what food they have consumed if they were asked in a questionnaire. Thank you for sharing this interesting article!
-
AngeliMalimban
It is amazing that in our day and age, there are so many pathways to receive information. Customers normally sign up for loyalty cards thinking about only the benefits that come to them (at least, this is how the stores sell their cards… that’s how I got suckered in to signing up for so many). However, it should be known that this data is used to help them decide what is best for their customers and the benefits that we get is how they get us to sign up. This is great how it helps find sources of foodborne disease outbreaks because as meggyli mentioned, it is hard to recall food from questionnaires, making it more time consuming to finding the cause of an outbreak. I just wonder if the customers were told that this is how the outbreak was determined before the article came out, and if they felt that it was a breach of privacy…
-
Ya Gao
It is such a clever way to use loyalty cards to investigate into food borne outbreaks! i never thought about this and never knew that they have my purchase history on file when I use my loyalty cards. Hepatitis A is not a trendy food borne disease in North America and vaccination is available to prevent the disease. But once it breaks out, I believe it could be a huge problem since it can transmit through close physical contact with an infectious person and the incubation period is relatively long. It is the quick action of the authority that stopped the situation from becoming serious. Using data from loyalty card to trace the source of an outbreak is a great tragedy to apply to future investigations.
-
-
laurenrappaport
Dangerously High Levels of Viruses in Olympic Waters
The upcoming 2016 Summer Olympics will be held in Rio de Janiero (Rio). Brazil is the first South American country to host the Olympic games. However, currently, the sanitation state of the city is creating major concern as it may interfere with the athlete’s safety to compete in some sporting events. Brazil has been facing sanitation issues with their water for many years now. Currently, the waters in which sporting activities will take place are filled with human feces and garbage putting athletes at a huge risk of illness and attracting infectious diseases such as norovirus or hepatitis A virus (HAV). 10,000 athletes and thousands of tourists will be gathering in Rio to take part in the Olympics next August. 1,400 of these athletes will be competing in sports such as rowing, canoeing, sailing, triathlons and long distance swimming, all of which will be experiencing high exposure to the contaminated waters.
An Associated Press (AP) analysis of the water quality from three Olympic sites was performed and revealed extremely dangerous levels of both viruses and bacteria. The test results showed that the virus and bacterial levels present in the water are 1.7 million times higher than what is considered a hazardous level in North America. The contamination is a result of household waste and sewage, which is unfiltered before entering the water streams. As the viruses present have low infectious doses, the concern for individual safety is on the rise.
An expert in risk assessment for waterborne viruses analyzed the results from the AP testing and estimated that athletes from around the world who are not commonly exposed to these viruses have a 99% chance of being infected by a virus via the consumption of only 3 tablespoons of water. This can cause severe sickness such as gastroenteritis, vomiting, and diarrhea. Furthermore, both viruses are easily spread from person to person creating the risk for large amounts of illnesses during this world event.
The major concern is for the athletes and the many tourists who will be gathering to watch the Olympic events. Both of these viruses are very easily attracted and spread. As such, the outcome of unsanitary waters could be catastrophic. Although Brazil committed to cleaning their water when they were selected to host the 2016 summer games, little improvement has been shown so far. Concerns have risen as now the games are less than one year away and little progress has been made. All individuals travelling to the games have been advised to receive heptatis A vaccinations however, little can be done about the prevention of norovirus. Therefore, the key solution to this issue is to clean up the waters by bringing the bacterial and viral levels down to a minimum.
Sources:
Associated Press (2015, July 30). Olympic athletes to swim and boat in “raw sewage”. CBC news. Retrieved from http://www.cbsnews.com/news/brazil-summer-olympics-water-contaminated-with-raw-sewage/
Brooks, B., Barchfield, J. (2015, July 30). AP Investigation: Olympic teams to swim, boat in Rio’s filth. Retrieved from http://bigstory.ap.org/article/d92f6af5121f49d982601a657d745e95/ap-investigation-rios-olympic-water-rife-sewage-virus
Centers for Disease Control and Prevention (2011, March 4). Updated Norovirus Outbreak Management and Disease Prevention Guidelines. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6003a1.htm
Hepatitis News (2015, August 21). Hepatitis A Concern fors for 2016 Summer Olympics in Brazil. Retrieved from http://www.hepmag.com/articles/hav_concerns_olympics_2831_27670.shtml
World Health Organization (2015, July). Hepatits A. Retrieved from http://www.who.int/mediacentre/factsheets/fs328/en/
-
catherine wong
This was an extremely interesting article. I did not know that Brazil had such problems in its waters, especially now when they are going to host the Summer Olympics in 2016. As we learned in class and as you mentioned above, these viruses such as Norovirus and Hepatitis A are highly infectious and could cause major consequences for the Summer Olympics when there are so many athletes and tourists from around the world all packed in those areas where the events are taking place. For Norovirus since it has such as high genetic variability and is very difficult for people to get immunity, wouldn’t people living in Brazil have a higher chance of getting ill with Norovirus compared to other countries with cleaner waters? I am actually quite interested to see if or how Brazil will try to clean up their waters before the Olympics and if they do not, what will happen to the athletes and tourists during that time.
-
ColleenChong
Hi Lauren, I have to agree with Catherine this is a very interesting article. I never knew that Brazil had such concerning sanitation issues, with high levels of norovirus and hepatitis A virus. This not only concerning for athletes but also the great amount of tourist that will be attending the events at the Olympics. The dense population at this event would serve as a large reservoir for virus, as mentioned in class, the incubation period can be up to 28 days. From Brazil the viruses can be affecting countries all over the world after the event due its long incubation period- causing a global outbreak. I think it will be extremely difficult to solve the problem that Brazil is facing, especially due to the fact that the viruses has many routes of transmission and its ability to survive. I am too truly interested in seeing what Brazil come up with to clean the waters.
-
TamaraRitchie
Awesome article Lauren! It is really important to think about all health and safety aspects when it comes to the Olympics. I had read previously that Brazil had a lot to do in order to be prepared for the summer 2016 Olympics, these articles focused mainly on drugs and crime though. I never thought about it through a food safety or health perspective. Having the Olympics in a developing country has it challenges as listed above. I am curious to see how they resolve this issue if they are able to. It seems it is a huge problem that will have to be resolved by fixing the sanitation program of the city as well as the safety of the water currently there. I am very interested to see what happens next summer, and if there are any Norovirus or other virus/bacterial outbreaks. Hopefully this is not the case as people will be travelling all over the world to enjoy the games. As well athletes would have trained for years to be given this opportunity and if they are not able to practice their sport in a safe and fair environment there could be negative backlash from the Olympic community.
-
amreenj
Really great choice of article Lauren! I have previously read about the sanitation issues present in Rio however I wasn’t aware of the shear magnitude of the problem. It is awfully concerning that the viral and bacterial levels present in the water are 1.7 MILLION times higher than what is considered acceptable in North America! I think that if Brazil is unable to get this water sanitation issue under control, they shouldn’t be able to host the Summer Olympics. Considering the low infectious doses of HAV and norovirus poses an enormous risk to not only the athletes but also to those visiting. The potential aftermath of such a large number of people getting infected is absolutely catastrophic! I really hope that Brazil takes control on the situation before the Olympics, although I am unsure as to how they will do this. It would require a major overhaul of their infrastructure which, I am not sure is possible in such a short time period.
-
mustafa akhtar
Brazil as a country is very big on soccer and it would be a national tragedy of the World Cup were to be moved to another country. This must be a huge concern! The whole event is dependent on healthy athletes.
-
JorgeMadrigalPons
the world cup happened last year… they are talking about the olympics
-
-
KristinaRichmond
This is an interesting topic, and I agree that contaminated water is a huge issue regarding the Olympics, but I was wondering what the consequences are for the population currently? How are residents and tourists using the water now? Hopefully with the Olympic pressure the time and money will be put into cleaning up the water and will be beneficial to the people living there in the future.
-
Michelle Ebtia
After reading this blog, I decided to do some more research on the topic, and found a few journal articles that have been investigating this problem. In one interesting paper by Fistarol et al. which has been published this month (November 2015), the authors had made a few suggestions and devised an action plan, which is inspired by what the Canadian government had performed to remediate Sydney Harbour in Nova Scotia starting in 2009. The authors point out that the most important change that needs to me made is the treatment of sewage from domestic residents (specifically slums) and hospitals, while keeping the polluters and stakeholders involved in the entire process, by making the findings and data on improvements available to the public. It is also of relevance to this course that even the fish that is harvested from this body of water is contaminated with pollutants and pathogens.
Work Cited:
Fistarol, G. D. O., Coutinho, F. H., Moreira, A. P. B., Venas, T., Canovas, A., de Paula Jr, S. E., … & Thompson, F. (2015). Environmental and sanitary conditions of Guanabara Bay, Rio de Janeiro. Frontiers in Microbiology, 6, 1232. -
Mandy Tam
Great Article!
I am surprised that there is no such standard on the relationship with the amount of virus that cause illness with water contact.
I think a lot of people do not know water is an important food source to be aware of as well. I guess probably because water is Canada is pretty clean, however, outbreak caused by water might increase in the future due to increase pollution to the water source. Therefore, this is something that we should seriously think about.
Anyhow, I am a person who like to drink water from the tab or directly from the stream when I am camping. Now I think I need to rethink again before I am drinking water from an unknown source.
-
cheryl lau
I agree with the comments above that it is surprising that the Olympic Committee chose Rio de Janiero as the location for the next summer games even with the current situation of the waters. Norovirus is especially concerning because there aren’t specific preventative measures that one could take knowing that they would be exposed to the virus. Although the effects of Norovirus usually presents with mild symptoms, this could be enough to affect an athlete’s health. It would be a shame for athlete who have been training for most of their lives to not perform their best and waste their efforts.
-
EmilyChow
Nice topic! This makes me wonder what regulations Brazil had in place in regards to water safety and also what changes have been implemented since it seems as though there are mainly preventative measures of making sure people receive vaccinations. Perhaps the contamination is worse in some waters than in others? Maybe the committee can focus on cleaning and regulating certain waters and coastlines in order to use their limited time and money most efficiently.
-
-
EmilyChow
China has Zero Tolerance for Listeria monocytogenes
Did you know that China has a zero pathogen standard that needs to be met for meat imports? Whether raw or cooked, meat and poultry from Canada shipped to China must contain no amounts of Listeria monocytogenes. How would this affect China’s food market and food availability?
Listeria monocytogenes is a facultative anaerobe, meaning that this bacterium is able to survive in environments absent of oxygen. It also has the capability of growing in temperatures ranging from 0 to 40 degrees Celsius. This allows Listeria monocytogenes to grow and to survive on refrigerated and frozen foods respectively. In Canada, presence of the bacteria on food is permitted as long as the detected amount is below 125 CFU/g for category 1 RTE foods and less than 100 CFU/g for categories 2A and 2B. These values were established because foods with less than these detected amounts of L. monocytogenes have low risk of causing illness. In fact, most foods consumed in Canada are usually tainted with L. monocytogenes. According to Health Canada, there is a 0-10% frequency of L. monocytogenes found in RTE foods.
Food from Canada that is exported must comply with the regulations of the country receiving the food, in this case, China. According to the China National Standards (GB 29921-2013), meat products cannot contain any amount of Listeria monocytogenes for every 5 samples tested. If meat and ready-to-eat (RTE) food producers want to export their products to China, they need to apply procedures that would completely eliminate L. monocytogenes from the food. To ensure that cross contamination does not occur, exporters need to follow proper equipment maintenance, sanitation, and handling procedures; however, this may be difficult for Canadian producers to achieve if we export our meat to countries with such requirements because meat can be contaminated through packaging and shipment processes. In addition, there is difficulty in eliminating the bacteria from foods due to the resistant qualities of L. monocytogenes such as sanitizer, acid, and desiccation tolerance, as well as its ability to attach and remain on surfaces.
China’s zero tolerance policy for the presence of L. monocytogenes in meat poses as an issue for other countries wanting to import their meat into China. If China buys meat from Canada and the meat gets tainted during exportation, China destroys the meat. This waste and reduction in food imports is not only harmful to both economies, but also to the food supply in China. Moreover, implementation and regulation of stricter laws is costly.
Compared to previous years, the presence of L. monocytogenes in foods has been increasing. The number of incidences of foodborne infection due to L. monocytogenes reported in China is similar to the numbers from different countries. Since China’s food market is rapidly developing, along with an increase in the population, there is a demand for pre-made, RTE foods. This increased consumption may also mean that there is more risk of infection, but there may also be a lack of supply due to the restrictions on imports. According to the WHO, the likelihood of developing listeriosis depends on multiple factors including how the food is stored, how many times contaminated food is consumed, and the amount of pathogen on the food. Rather than having the zero tolerance policy, perhaps China can consider educating consumers on basic food safety principles.
Considering the risk of infection and the loss of trade, do you think the zero tolerance policy is necessary?
Works Cited
China National Standards (26 Dec 2013). Food Safety National Standard Limit of Pathogens in Food Products. Retrieved from http://cexgan.magrama.es/MODULOS05/Documentos/GB29921-2013-PatogenosEnAlimentos.pdf
Feng, Y., Wu, S., Varma, J. K., Klena, J. D., Angulo, F. J., & Ran, L. (2013). Systematic review of human listeriosis in china, 1964–2010. Tropical Medicine & International Health, 18(10), 1248-1256. doi:10.1111/tmi.12173
Health Canada (1 Apr 2011). Policy on Listeria monocytogenes in Ready-to-Eat Foods. Retrieved from http://www.hc-sc.gc.ca/fn-an/alt_formats/pdf/legislation/pol/policy_listeria_monocytogenes_2011-eng.pdf
Wu, S., Wu, Q., Zhang, J., Chen, M., Yan, Z. A., & Hu, H. (2015). Listeria monocytogenes prevalence and characteristics in retail raw foods in china. PloS One, 10(8), e0136682. doi:10.1371/journal.pone.0136682
-
yichen25
I personally think that the zero tolerance policy shouldn’t be enforced in China. There are definitely some pros and cons when it comes to zero tolerance policy of Listeria monocytogenes. The pros being that the meat that arrived in China is much safer for consumption as there are no traces of Listeria monocytogenes, which further decrease the risk of foodborne diseases. However, in this case, the cons outweigh the pros. This is because the implementation of zero tolerance policy will result in less international meat trading between China and other countries and also contributes to more meat wastage as all the imported meats that doesn’t fulfill the requirements will be sent for disposal. China should definitely consider loosening their tolerance policy for Listeria monocytogenes to find a balance that will benefit them the most.
-
JorgeMadrigalPons
I agree with yinchen25. China may be loosing more with this zero tolerance policy. Population in China is really large, thus they must have an efficient food supply system. I think it could be better if the Chinese government focused on informing its citizens about the potencial problems of eating RTE. It is known that Listeria monocytogenes tends to target immuno-compromised individuals, like children, pregnant women, or elderly people, therefore, I think that cutting RTE meats from these individuals diets could prevent potential infections.
-
angel519
I am surprised to know that China has such a strict policy on import meat produce. I think having a zero tolerance for Listeria monocytogenes is a good approach of preventing foodborne illnesses caused by L.monocytogenes. However, since the number of incidences in China is similar to the numbers from other countries, the governmnet should pay more attention on inspections of post-import activities such as transporting and processing. Even if the imported produce has no L.monocytogenes, inappropriate manufactor practices will introduce the pathogen to the produce. The whole process from import to consumer should be inspected and regulated strictly to be able to achieve zero tolerance and reduce in L.monoctyogenes induced illnesses.
-
DeniseZhang
I am from China and I did hear a lot of food safety issues in China these years. Maybe it’s due to this “zero tolerance policy”, Listeria is actually not the most reported cause of food-borne illness in the news that I have heard of. I do think a strict regulation is necessary, as there are more and more food safety issues are revealed and reported, food safety becomes a big concern to most of Chinese, as least to those who care about the quality and the safety of the food. After years hearing sever consequences caused by unsafe foods, people were kind of scared and try to seek out foods that come from more reliable source. Therefore I think a strict regulation on Listeria can provide a safety barrier for people in China not just physically but also mentally. Yes, there might be loss in economics, (please don’t judge) but I think food safety is more important for people.
-
wen liao
It is very interesting that China has such a strict policy on L. monocytogenes while China is one of the countries that has the most food associated outbreaks. However, I do think that it is a good policy especially considering the current status of Chinese food industry. In China, there are many aspects of food production and processing that is not strictly supervised and controlled, which lead to a lot of foodborne outbreaks that should be avoided. For example: the melamine adulteration in infant formula posed a large scandal over Chinese milk industry. Although it is a very strict rule that L. monocytogenes is zero tolerated in China, I have to say that it is better to be safe than sorry.
-
NorrisHuang
I kind of have mixed feeling about this “zero tolerance policy” because it is being enforced in China and still China has similar number of listerosis cases as the other countries, wouldn’t it be worse if this policy is no longer administered? But I also agree that this policy does affect international trade. Grew up in China, I don’t think much of the food safety cases are related to microorganisms. More of them are related to food adulteration and addition of illegal food additives. And I am also surprised to know that China has such a strict policy on microbial aspect of imported food.
-
Michelle Ebtia
This is certainly as good as it can get in terms of food safety and risk elimination rather than mitigation. However, as noted by other readers, the costs associated with this policy might outweigh the benefits, e.g. loss of trade. Also, from an international trade perspective, one might wonder if this policy is in place in an attempt to limit the RTE import to china, for example in support of local food production. This assertion might be backed up by a study (Shi et al. 2015) that found 6.87% of RTE food samples in China are contaminated by Listeria anyway!
Work cited:
Shi, W., Qingping, W., Jumei, Z., Moutong, C., & Zéan, Y. (2015). Prevalence, antibiotic resistance and genetic diversity of Listeria monocytogenes isolated from retail ready-to-eat foods in China. Food Control, 47, 340-347. -
teewong
I can understand where China is coming from when they imposed the zero pathogen tolerance policy on import foods. RTE foods stand for “ready to eat”, meaning no prior preparations (ex. thermal processing, freezing) are needed prior to consuming, therefore, the chances of getting infected from eating RTE foods are very high! I agree with @emilychow that China should enforce more on educating the public more on food safety preparations, however, in RTE foods, there is really very little we could do to eliminate the pathogen since they are way too tiny to be seen with bare eyes. The most we could do is to throw away the product if it looks spoiled. Listeria monocytogene is also a tricky pathogen since it could grow at refrigerated temperature. I feel it is totally reasonable that they pose a food safety regulation on imported foods.
-
-
mustafa akhtar
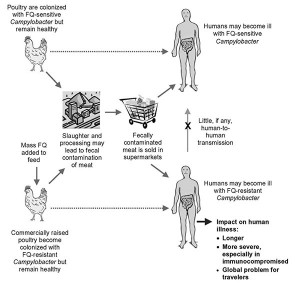
Football team and friends at Durand High School effected by Campylobacter Jejuni
September 24, 2014: At least 22 members of the football team were reported sick, some hospitalized, after the team potluck at the Durand High School in Wisconsin. Lab tests have confirmed suspicions of the pathogen to be Campylobacter Jejuni. Wisconsin Department of Health said that unpasteurized milk served at the dinner was the cause of the outbreak. More than 50 Durand High school students were forced to stay home due symptoms that included Diarrhea, cramps, fever, and stomach pain.
Read more about the news break here: http://www.weau.com/home/headlines/NEW-INFORMATION-Campylobacter-infection-found-in-one-Durand-patient-276958321.html
The potluck is a yearly tradition at the high school usually held at the nearby school. Dinner included Chicken Alfredo, Kool-Aid, water, and raw milk with chocolate syrup added.
The Wisconsin Department of Health (DHS) interviewed all players and coaches of the football team (ill and unwell) in order to assess symptoms, as well as find the root of the problem. Consumption of raw milk appeared to be the isolated as the only food item associated with the illness. Symptoms lasted for about a week and ranged from mild to severe. Other complications include meningitis, urnary tract infection, arthritis, and sometimes, Guillian –Barre syndrome.
One of the students, Brianna, reported unusual pain in her hips and knees, limb weakness, as well as numbness for which she was hospitalized.
Reportedly, other students were hit hard by the symptoms as well, many suffered from bloody diarrhea and noticeable weight loss.
More about the investigation:
http://www.jsonline.com/business/raw-milk-blamed-as-38-at-durand-high-football-potluck-are-sickened-b99390272z1-282848161.htmlAccording to the Health Canada website, people infected with C.jejuni can experience an array of symptoms. Some may not get sick at all, but still be able to spread the disease. Others may experience a severe flu, while some may be hospitalized.
The outbreak affected the football team so much so that the high school cancelled the Sept 27th football game against Amery High School.
Campylobacter Jejuni, the pathogen identified as the cause of this outbreak, is found in digestive systems of cattle, poultry, and animal feces. The DHS collected samples of manure from the farm where the raw milk was produced, and the bacteria strain was found positively correlating the bacteria to the illeness. People with weakened immune systems are at a greater risk of complication including arthiritis, meningitis etc.
Public Health Canada website:
http://www.phac-aspc.gc.ca/fs-sa/fs-fi/campylo-eng.phpThe state-law prohibits sale of unpasteurized milk products to the public to contain bacteria that may promote food borne illnesses. Moving forward, the school recommends fewer dinners like potlucks, as the food quality is difficult to control. The effects of this have been particularly eminent to the student population.
-
ayra casuga
Nice blog! It’s really sad when you hear stories about school-related events get affected by food-borne illness outbreaks and yet it occurs so frequently. I think its a good idea to ban the sales of unpasteurized milk in secondary schools because it may not be handled/distributed safely because the people in those events may not be aware/or taught how to ensure food safety in those products. In addition, some students may be highly sensitive to unpasteurized milk and these types of issues really reflect on the schools policy.
-










Reply