I started volunteering at Headway in May 2013. Activities-wise, I usually help with the art classes and music therapy or accompany the members on the walks to Granville Island. I wish to share with you three things I’ve learned at Headway that changed how I understand brain injury.
1. Focus on empowerment for healing
We’re accustomed to view individuals with brain injuries as being disabled and somehow less than everyone else. But you never see that we feel sorry for you vibe at Headway. Everyone, including the staff, is seen as equals. No one is being treated or “fixed” for their impairments.
Instead, Headway aims to provide social support and empower members to set/work towards their personal goals and live the best life that is possible for them. This may sound abstract and cheesy, but it’s not all just talk— we follow up! In fact, Headway uses software called ShareVision to document personalized member goals and track individual progress. Below is a short descriptive video of this program.

2. Dramatic fluctuations in mood states
Perhaps most striking is seeing how differently a member can behave from the week-to-week that I volunteer. For example, I work closely with a member who is on most days gentle and polite. We would play Wii Golf and laugh whenever our shots would land far from target. Other days, this member would be aloof and irritable. On these days, he would curse loudly whenever he did not make a good shot in Wii Golf.

The changes in this member’s mood is so severe that I often feel like I’m talking to someone entirely different. (Image via Wikipedia)
Connecting this to our class discussions on assessment, I can appreciate how difficult it is to gain an accurate clinical picture of a patient’s condition. A study by Chamelian et al. (2006) found that TBI patients with depression do worse in measures of memory, attention, and executive functions. The current convention of conducting neuropsychological tests in one long day clearly isn’t ideal, but neither is overwhelming patients with tests too frequently. I wonder what the right balance is.
3. Prominence of social factors
One of the most emotional experiences I had volunteering was a conversation I shared with a stroke survivor. She was telling me how the most difficult part of her brain injury is not dealing with her neurological impairments. Rather, it was the crushing guilt of being a burden to her family. For a long time, she told me how she painfully hated herself for needing to depend on her family for financial support.
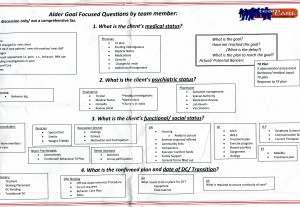
Her story was on my mind during Jessica’s facilitation on how TBI can affect social dynamics. Clearly, these social changes (besides physical symptoms) can also have profound effects on an individual’s well-being. These factors are an important part of case management. When I sat in during rounds at Langara hospital, functional/social status was a very important part of the meetings (see below).

3 responses to “How Headway has changed my understanding of brain injury”