During the first semester of my fourth year, the main clinical examination was the Process of Care or “ADPIE” assessment. The client chosen as the ADPIE had to meet a few criteria, including being P3/P4 perio status, requirement of images to supplement assessments, and requirement of local anesthesia in minimum of one area for debridement.
The client I had chosen was a P4 client who had not seen a dental professional for two years prior to seeking treatment at UBC.
She is a 72 year old woman who presented with controlled high cholesterol and hypothyroidism. At initial assessments, her periodontal pockets ranged from 5mm-8mm.
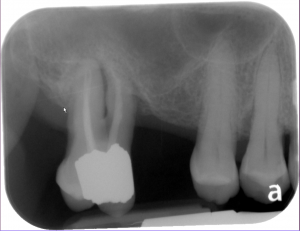 Radiographs revealed generalized horizontal bone loss and areas of vertical bone loss, and mobility in several areas, notably 18.
Radiographs revealed generalized horizontal bone loss and areas of vertical bone loss, and mobility in several areas, notably 18.
Treatment plans involved full mouth debridement using local anesthetic, stain removal, and fluoride application. Promoting self care was emphasized with this client as she was willing to make the necessary changes to improve her oral health, but did not have the knowledge to do so. Lessons emphasized cleaning specific “tough” areas in the mouth, such as the class II-III furcations on 18 and the 44-47 bridge, as well as generalized oral health instruction on flossing and brushing techniques.
Overall, this client proved to be a challenge for me. Although I felt competent in my clinical skills, there was much to be learned from this client. I was able to gain confidence and experience with providing local anesthesia for debridement for this client as it was required for the majority of the dentition, and it was especially challenging as she had irregular anatomy. Due to the recession, furcations, deep pocketing, and other issues present, I learned to use a variety of instruments that I previously did not feel confident in using. I was able to finish the appointments in less time than I had planned for because of these skills I had gained. In addition, I was able to build rapport and trust with this client, despite an existing language barrier and the client’s low oral health literacy.
I was very pleased to see many improvements in the client at the re-evaluation and recall assessments. There was a reduction in plaque accumulation, BOP, and pocketing. She had become confident in her oral hygiene practices and it was evident that she had made a conscious effort to improve her oral health. As much as I was glad for her oral health successes, I am even more so grateful for how she helped me as improve as a clinician.




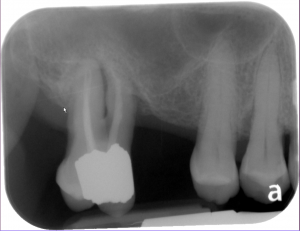 Radiographs revealed generalized horizontal bone loss and areas of vertical bone loss, and mobility in several areas, notably 18.
Radiographs revealed generalized horizontal bone loss and areas of vertical bone loss, and mobility in several areas, notably 18.