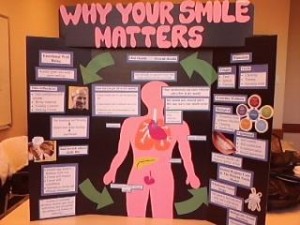
Figure 1. This is the table clinic my group and I made.
At our externship sites in term 1, my group and I had our first exposure to the mental illness population. It was apparent that both Pioneer and Lina’s place had immense need for oral care. Upon completion of the situation analysis, review of the literature and assessments we were able to piece the puzzle together. One of the most predominating factors would be the lack of self-esteem and lack of motivation present in this special needs population. (1) As a result, our group decided to promote oral self care behaviour that tailors to the resident’s motivational and self-esteem. As these homes are transitional homes, we promoted the relevancy of taking care of their oral health to the advancement of the next stage of their lives. We talked about how research having disease free mouth was related to more smiling and more smiling was related to higher self-esteem.(2,3) Not only did we promote oral self care practices using psycho-social factors, we talked about overall well-being. As a result of our table clinic the residents were engaged and asked a lot of questions and some of them express that they did not know about a lot of the knowledge that we shared with them.
Please see the attachment for our pamphlet that accompanied the table clinic.pioneerpamph
Reference
- Griffiths J et al. Oral health care for people with mental health problems: guidelines and recommendations. Report of BSDH Working Group. British Society for Disability and Oral Health. January 2000.
-
Patel RR, Richards S and Inglehart MR. Periodontal Health, Quality of Life, and Smiling Patterns – An Exploration. J Periodontol. 2008;79:224-31.
- McKeown L. Social relations and breath odour. Int J Dent Hyg. 2003;3:213-7.