INCEPTION
I love in passionate people the mutual ease with which a grand plan is hatched.
I received an email some months back from just such a person, a normal email requesting a PDF of a paper, which quickly blossomed into a conversation on shared interests, specifically aspects of cerebral blood flow (CBF) and its regulation during prolonged apnea in breath-hold divers. Prof Zeljko Dujic is one of the world’s greats on all aspects of diving (amongst other things) and is motivated, to say the least. Now I’d love to say that I immediately associated the Dujic name with all of his key papers and findings but that would be a lie. Rather I quickly perused the papers I vaguely recalled and got the email conversation rolling… and a good thing, because the project we ended up recently completing was in every sense amazing.
Why are breathe hold divers so interesting? Basically because they can do something that no one reading this is able to do (unless you happen to be a breathe hold diver, I suppose). “Prolonged apnea” is a relative term, in my case a whopping 90 seconds (maybe), but in these athletes the act is a very different story, and a very interesting physiological phenomenon. Training for a variety of events ranging from static apneas whilst floating face-down in a pool (current world record: 11 minutes 35 seconds!) or No-Limits where using a weight to descend well past the photic zone of the sea, and a balloon to return to the surface (current record: 214m!) such athletes can remain conscious into levels of hypoxemia much lower than the average person can endure – meaning that if you attempted such a study (not that you’d get ethics to do so) with the use of a thick plastic bag and your fellow grad students there’d likely be a few fewer grad students standing around drinking coffee. Herein lies the tremendous opportunity to study in Prof Dujic’s lab, along with Croatia’s national apnea coach Ivan Drvis, and his athletes.
THE PLAN
My interest (and thesis) is in the regulation of cerebral blood flow, particularly in the context of this regulation by changes in arterial blood gases (oxygen and carbon dioxide). During a prolonged apnea, arterial content of O2 decreases and CO2 increases — each of which drive vascular dilation in the brain and a consequent increase in CBF. During a prolonged apnea in a trained apnea diver, arterial blood gases change far more than in any conventional setting, indeed, far more than can be driven experimentally in the lab (or at least what can ethically be achieved in the lab, clearly its possible to give someone pure nitrogen to breathe). In fact these divers don’t breathe for so long that were they an average person to breath-hold that long (read: duct tape), the O2 content in their blood would render them unconscious very quickly; ergo, these divers must adapt, of have adapted, or perhaps be predisposed to such tolerance. So on the one hand these athletes are not “average” people – not the usual “random sample” – but this is precisely what makes them so fascinating: their peculiar tolerance to hypoxia.
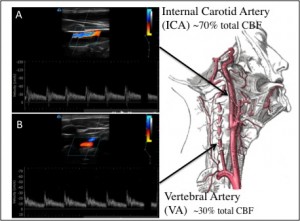
Fig. Schematic depicting gold-standard measurement of cerebral metabolism. Duplex ultrasound of the (A) ICA and (B) VA for regional CBF quantification, that, combined with measures of brain venous blood from the IJV.
Because different areas of the brain are responsible for different functions, and because some of these functions relate to cardiorespiratory regulation (i.e., heart, blood pressure and breathing), regional differences in blood flow in the brain is of interest during any challenge to the cardiorespiratory system – such as exercise, orthostatic changes (e.g., standing up from sitting), myriad disease states, or…. breath-holding. It would be therefore be interesting enough to study regional CBF (using Duplex ultrasound of the internal carotid and vertebral arteries, see Figure) during a prolonged apnea, but our plan goes further.
I should digress at this point and address one of the fun sides of science – the continually evolving idea, which gives the continually evolving plan, which if you’re not careful will typically manifest in the ridiculously complicated multi-hypotheses 5-hour protocol that cannot possibly be completed in less than 8 hours. Now I call this a fun side of science because I like a little chaos – if everything is so obviously feasible and there’s no chance of something going wrong than where’s the excitement in that? Human physiology is full of these things – the human element twice over: once from the physiologists who want to answer as many questions as possible in a given experiment, once from the consequent requirement for a large research team, and once more because you’re studying people. I suppose that’s three times the human element, the more the merrier. But fast-forward a couple months and the day of the study we finalized the protocol to a much more simple format – that which I describe here – focused on two distinct hypotheses. In the end you must get as much out of a study as possible, but not so much you get nothing!
Another characteristic of breath holding is that if the apnea is sustained long enough the respiratory muscles begin to contract involuntarily. These involuntary breathing movements (IBM) seem to augment CBF during a breath hold – each contraction produces a surge in venous return, cardiac output and arterial pressure and CBF gets a transient boost too. Now this may be good for cerebral oxygenation but to know the effects of IBM per se you must isolate the effects of the apnea induced changes in blood gases from the apnea (and consequent IBM). Another issue is that blood gases are often estimated from end-tidal gases – a sample of gas at the very end of an expiration that largely reflects the partial pressure of the blood leaving the alveolar vasculature (arterial blood). Clearly this presents a methodological problem if the subject is holding their breath… enter rapid arterial blood sampling.
We insert a catheter into the diver’s radial artery and take a small blood sample each 30 seconds of the breath hold. To assess the effects of apnea and IBM versus the hypoxia that results from apnea we will use a system (the ‘AirForce’; thanks to the computational genius of Dr. Glen Foster) that adjusts the inspired fractions of O2, CO2 and N2 to “target” a specific arterial blood gas profile – as close as possible to the same profile elicited during each person’s own apnea. Beautiful!
EXECUTION
Because we decided to use the AirForce, and because we wanted to measure flow through both the internal carotid and vertebral arteries, and probably also because Prof. Phil Ainslie wanted another student somewhat less manic than me (never a bad plan), Anthony Bain was invited. Now given that Tony has enough going on at the moment to keep him busy with twice the hours in the day, and given that he ended up being totally instrumental to the study’s success, I owe him an unprecedented amount of beer. A pity he will no doubt at some point read this ‘blog’.An equally fortuitous addition to the team was Dr. David Macleod – anesthesiologist at Duke Medical Clinics, NC, USA. David is an outstanding individual who can tell a story as well as he inserts a jugular venous line (we know, we’ve received both) and who’s calm, commanding demeanour is the type you have faith could not be rattled – which is especially comforting if he happens to be placing a catheter in your neck at 5050m in Nepal…
I hate packing. When we went to Nepal a year ago or so I theoretically headed all the packing from the UBCO side (I say theoretically because there were plenty of heads looking over my shoulder, and for good reason too, there are practical reasons of competency I hate packing) and managed to not forget anything crucial. I make lists. Iterations of lists that are revised, finalized, printed and finally ignored. I am the same with packing for climbing trips… I can have lists with all necessary items but come packing time I need to see everything laid out in front and gauge from there if I have everything needed. Totally illogical and wrought with problems but with Tony’s help we managed to forget nothing essential. Phil, Tony and I packed all these items – basically an entire lab – into the well-used Pelican cases and we headed to the airport. Twenty-four hours later we rolled off the plane into Split, where fortunately Zelko was waiting to talk the customs agent into letting us through unmolested with a more than $200K in equipment. A couple hours later we were tucked into our Monastery beds for a few hours of sleep before our jet-lag woke us up at 4 am. Wait – Monastery? Originally Zeljko set Phil and I up in the rooms across from his lab but through the planning process when first Tony and then David was added to the roster we needed more space. A 10-minute walk from the lab is a Monastery (the kind with Monks… A rather large language barrier and an unfortunate ignorance of religions in general on my part preclude further detail on the topic. They do supply some excellent wine, however) on the top floor of which we were housed.
Our windows looked into the back courtyard and garden of the neighbouring house: olive and pomegranate trees, rows of veggies, and the odd vestigial farming remnants decaying into the ground. Between us and the mountainous Dalmation coastline running south in a craggy crescent of white limestone, arid scrub brush juxtaposed against the blue Adriatic Sea, are the porous concrete blocks of government-built apartment buildings typical of Eastern Europe, the residual architecture of a recently socialist country. The sunrise basks the islands to the west in hard orange and I look forward to getting caffeinated.
 Ivan Drvs is the Croatian national apnea coach and has handled all of the subject recruitment. Getting volunteers for a study is an obviously pivotal aspect of every study and typically takes up a disproportionate amount of time; Ivan’s participation was totally essential to this study. Over the 12 days of data collection only one subject cancelled, and fortunately this was on the first day because it took the entire day to set up the lab. This basically consists of plugging everything in, getting Labchart (the data collection software) set up and calibrating the AirForce but there are always obstacles. Phil and Tony took care of the latter two – no small feat – and we were good to go by the end of the day, and had time for a quick tour of the nearby neighborhood next to the coast.
Ivan Drvs is the Croatian national apnea coach and has handled all of the subject recruitment. Getting volunteers for a study is an obviously pivotal aspect of every study and typically takes up a disproportionate amount of time; Ivan’s participation was totally essential to this study. Over the 12 days of data collection only one subject cancelled, and fortunately this was on the first day because it took the entire day to set up the lab. This basically consists of plugging everything in, getting Labchart (the data collection software) set up and calibrating the AirForce but there are always obstacles. Phil and Tony took care of the latter two – no small feat – and we were good to go by the end of the day, and had time for a quick tour of the nearby neighborhood next to the coast.
Our first subject on Day 2 was Goran Colak who a week prior had broke the world record for an O2-assisted static breath hold: he breathed pure oxygen for around 20 minutes and then held his breath whilst floating face down in a pool for 22 minutes! Colak (pronounced Chol-ack) is quite a sensation in the free-diving world at the moment, and arrived with a documentarian cinematographer who was producing a film about him. Perhaps for good reason as he seems to break every record he goes after, and anyway, held his breath for 7 minutes 45 seconds. Quite the first subject.
There are always teething issues in every study but with a few minor mistakes during this first test the rest of the study really went very well. We tested a minimum of two people each day completing a total of 17 tests by the end of 12 days. Seven of these were replicated in the same individual after they had consumed indomethacin – a prostaglandin inhibitor that reduces cerebral blood flow by about 30% – allowing us to assess the role of CBF per se in breath hold time and response to progressive hypoxia.
The photos and captions below should give a better idea of what data collection was like:
- The experimental set up. Clockwise from left: Ivan Drvis, coaching the subject through the breath-hold; Phil Ainslie, watching the data come into LabChart he is responsible for the timing of the experiment, ensuring everything is running (you would be surprised how easy it is to ruin a trial by forgetting to turn on the finipres measuring blood pressure), and communicating between the scanners, blood extractors, and Ivan; Dennis Madden, Zeljko’s PhD student expert in SCUBA diving physiology, Petra Zubin, MD and soon-PhD of diving physiology; Chris Willie (me) measuring vertebral artery blood flow; Anthony Bain measuring internal carotid artery flow.
- By the end of the breath hold every athlete is at his or her limit; maximum apneas require a great deal of psychological resolve.
- Radial arterial catheter for repeated sampling of arterial blood.
- Hypoxia is profound when its color shows the desaturation of arterial blood!
- End of apnea (left) versus pre-apnea.
Having just returned from the trip I now face analysis. We analyze our ultrasound videos using custom software that tracks the vessel walls of the artery we scan, but this process takes about 3-4 times as long as the length of video. Suffice to say I have many late nights ahead… But before we headed back Tony, Phil and I spent two days climbing on Hvar Island off the coast of Split. Beautiful conglomerate cliffs with chunks of polished marble made for technical steep climbing and we swam in the clear the Mediterranean and drank the local Ojusko to cool off in the evening.
In sum, the trip was a tremendous success. We collected what are probably the most hypoxic arterial blood samples ever collected in healthy humans (including some collected above 8000m!) and had some fun doing it, started what looks to be a great collaboration with Prof. Dujic’s lab, and finally enjoyed a few days climbing and relaxing in a beautiful place.
In the coming weeks I will be putting my head down to complete the data analysis and then write the manuscript as I aim to finish my PhD by the spring.
–Chris Willie, PhD Candiate









