Can bacteria now consciously make the decision to change its’ shape to avoid being targeted by antibiotics? This article titled “Bacteria caught changing shape to evade antibiotics” seems to think so. However, upon reading this article, I discovered that it’s not that the bacteria makes the conscious decision to change its’ shape in order to avoid being targeted by antibiotics, but rather, the environment that the bacteria is in allows it to shed its’ cell wall. The title of the article is extremely misleading, and can cause undeserved panic because it is implying that bacterial organisms that are damaging to humans have evolved to the point where humans can no longer control them.
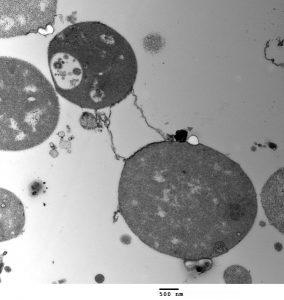
TEM of L-form bacteria from Mark Leaver of Newcastle University
If you continue to read the article, you’ll also discover that this certain strain of bacteria can’t evade all antibiotics. It can only make antibiotics that target the cell wall of the bacteria ineffective. There are antibiotics specifically made for targeting cell walls because there aren’t any human cells with cell walls, which makes it easier for the antibiotics to target the right cell. However, bacteria can shed its’ cell wall under non-hostile conditions such as an environment with high sugar concentration. By shedding that wall, the bacteria makes itself harder to detect by the antibiotics and our own immune system. That means that there is one less thing to differentiate the bacteria cell from our own human cell.
With a strong and healthy immune system, the L-form bacteria can eventually be destroyed. It is a little bit more complicated for people with weaker immune systems because they need help from antibiotics, but the antibiotics are ineffective because bacteria will stay in their L-form until the antibiotics leave the system, in which case the cell wall forms again.
Ultimately, there is no need to be worried that bacteria have evolved to consciously change its’ shape to avoid being targeted by our immune system or by antibiotics because it doesn’t. All the bacteria is doing is performing the functions it is programmed to do, like setting up protection against a hostile environment whether it is with a cell wall or without one.
-Sharon Li


