In beautiful British Columbia, we are surrounded by mountain ranges everywhere you look. How did they get there? Seems pretty straightforward right? We learned about this in school. Two tectonic plates smoosh together like two pieces of paper and a mountain range rises up in the middle. But what if there is a mountain range smack dab in the middle of your tectonic plate? How did that get there? Maybe mountain ranges are not as easy as we thought…….

Source: https://commons.wikimedia.org/wiki/User:Gorgo
Turns out that mountain formation is not so straightforward, it can depend on the thickness, strength, and density of a tectonic plate. Tectonic plates can collide, but they can also move apart from each other, sideways with each other, or underneath one another. Luckily, we have geologists like Dr. Saylor to help us figure these things out. Dr. Saylor is an expert in reconstructing the formation of mountains, and this past year, amid shutdowns due to the pandemic, Dr. Saylor and his team attempted to solve the enigmatic Laramide ranges. The Laramide ranges are an isolated mountain range in the middle of the North American plate. With no surrounding plate that could have collided and caused this formation, the Laramide mountain ranges have stumped geologists for years. By using computer modeling in this study Dr. Saylor and his team were able to reconstruct the exact thickness and strength of the tectonic plate that resulted in these formations almost 80 million years ago. They were then able to model how this tectonic plate might have buckled in such a way resulting in the formations we see today.
As someone from the general public, it can be hard to visualize how this study and its findings can affect us in our daily lives. In order to see the bigger picture, we asked Dr. Saylor what his study and others like it can mean for the general public.
To learn more watch the video below.

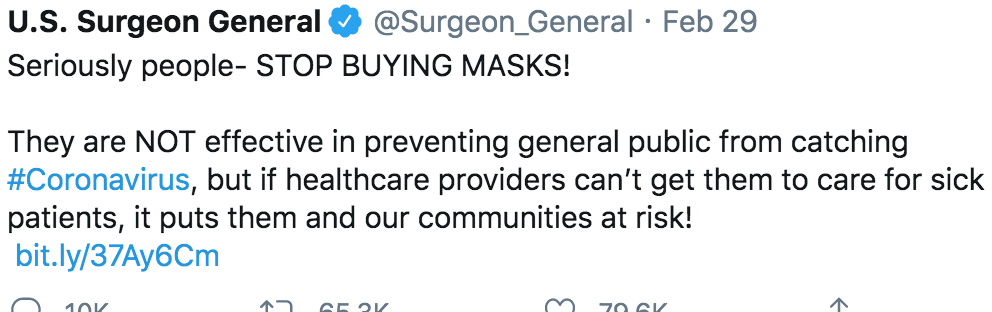
When we asked Dr. Saylor about the timing of this study and the COVID-19 pandemic he chuckled and replied “Yup, this is a COVID project”. Dr. Saylor is not alone; many researchers across all fields have felt the effects of the shutdown. We wanted to get a peek behind the curtain and ask a scientist currently doing research how they were affected. Listen below to hear how that interview went.
About Joel Saylor
Joel is currently an Assistant Professor here at UBC in the Department of Earth, Ocean, and Atmospheric Sciences. Joel received his Ph.D. from the University of Arizona and has spent time doing fieldwork in Peru, Bolivia, Columbia, and Tibet. Currently, the computer modeling Joel used in his study is being used to map other parts of the US and Canada and Joel has hopes of a global application of the computer modeling used in this study.
To learn more about Joel Saylor and how to get in contact with him check out his website
Written by Dylan Chambers, Selin Acikgoz, Ryan Reiss, Garangda Awar Mabior