Have you found yourself constantly checking your phone when someone likes your post or sends you a message? Then you might have what is called “social media addiction”.

Tiktok, an example of a popular social media app. (via Wikimedia Commons)
How does Social Media Addiction work?
Cognitive neuroscientists have shown that rewarding social stimuli – positive feedback by our peers, messages from loved ones – activate dopaminergic reward pathways. Dopaminergic reward pathways are pathways that release the neurotransmitter dopamine, a molecule that causes pleasure. The brain has three major dopaminergic reward pathways, the nigrostriatal, the mesocortical, and the mesolimbic system. These pathways are activated when a user receives social stimuli on social media, specifically a notification. Therefore, this is why when you receive a notification, you experience a feeling of pleasure.
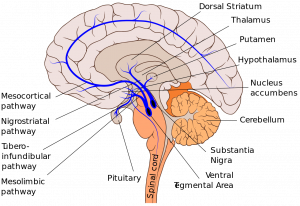
Dopamine pathways in the brain labelled as the mesolimbic, nigrostriatal, and mesocortical pathway (via Wikimedia Commons)
When talking about social media, Facebook, Snapchat, Instagram, Tiktok are all prominently huge social apps that many teenagers/young adults use. Every notification from social media apps like these, whether it’s a message, a “like” on Instagram, or a Facebook notification is scheduled on a variable reward schedule, introduced by psychologist B.F. Skinner. These apps are designed with the schedule in mind to maximize dopamine release, producing addictive tendencies similar to gambling and recreational drugs like cocaine to keep users using their products as much as possible.
How can I tell if I have social media addiction or will be likely to be addicted?
Addiction is normally classified as “engagement in the behaviour to achieve appetitive effects, preoccupation with the behaviour, temporary satiation, loss of control, and suffering negative consequences.” In the context of social media addiction, it would mean users would be:
- Consistently checking our phones to engage with social media apps.
- Only feeling satisfied when we engage with the apps.
- Suffering negative feelings when using or not using social media.
As well, a study demonstrates that users that struggle with “fear of missing out” (FOMO) behaviours predicted social media addiction. Additionally, it is also noted that attachment anxiety and avoidance predicted social media addiction, but this relationship was no longer significant after the addition of FOMO. Furthermore, the study finds users who display extraversion and neuroticism are more likely to use social media in the first place.
What does this mean for me if I’m addicted?
Social media addiction can lead to lower self-esteem, where low self-esteem is associated with lower satisfaction with life. Consequently, due to low self-esteem, it was further found that social media addiction was affecting depression indirectly. Many users suffering from social media addiction also found themselves experiencing time distortion, where those who were addicted were more likely to present significant upward time estimate bias. Additionally, the following Ted Talk by Bailey Parnell further highlights social media and its role in causing a poor mental health state.
Preventative Measures
 Curing social media addiction is hard. As previously mentioned, companies that make the apps we use purposely design their apps to maximize the use of our dopamine-driven reward circuitry to keep us continually using their apps. Seemingly, the only way to cure the addiction is to simply stop using the apps, and remove them from our phones.
Curing social media addiction is hard. As previously mentioned, companies that make the apps we use purposely design their apps to maximize the use of our dopamine-driven reward circuitry to keep us continually using their apps. Seemingly, the only way to cure the addiction is to simply stop using the apps, and remove them from our phones.
Martin Au-yeung