Introduction:
For Week 3, Assignment 1:3, our team was instructed to create three definitions of a relatively complex term used in our profession for audiences that may not have experience in this field. This aids our understanding of the importance and role of definitions in technical writing. Additionally, this assignments support with clarifying and
With a growing background in healthcare, medicine treatment, and sociology, I explored the intersection of these three constructs and focused on health equity due to its dynamic and important nature impacting society. The intended audience for this definition includes a general population that may not have exposure to health education and may have higher health equity in their own lives. This intended audience will grow more conscientious of the barriers that exist to inhibit health equity in their surroundings.
In the submission below, I have outlined three different definitions for health equity. Firstly, I will define health equity with a parenthetical definition. This definition includes a synonym or a clarifying phrase in parentheses following the term. The second definition will include a sentence definition, which expands upon the parenthetical definition by providing the broader class and noting distinguishing features of the term. In conclusion, I will define the term health equity with an expanded definition that includes the history, operating principles, required conditions, and negation of the term in its use and space in society.
Parenthetical Definition:
Within our modern society, health equity (an individual’s access to sustainable, accessible health and wellbeing) is variable across the general population and is heavily influenced by an individual’s social determinants of health.
Sentence Definition:
Term: Health equity
Class: classification of sociomedical wellbeing of an individual
Distinguishing features: accessibility to achieving adequate and sustainable social determinants of health leading to fruitful vitality.
Full Sentence Definition: Health equity, which can be used to determine the sociomedical wellbeing of an individual, includes classifying an individual’s accessibility to achieving adequate and sustainable social determinants of health leading to a full, fruitful life.
Expanded Definition:
History:
Health equity evolved from research conducted by sociomedical philosophers and scholars as early as the 18th century, including academics such as Fredrick Engels and Rudolf Virchow noting how class inequities lead to inequities in health (Fee & Gonzalez, 2021). Health equity was not acknowledged in its full nomenclature until late 1970’s, when the World Health Organization held a conference towards advancing health education access across the world.
Researchers encouraged academics and healthcare professionals to open their eyes at visible and invisible barriers for individuals with disadvantaged social determinants of health. This conference, also referred to as the Alma-Ata Declaration of 1978, has had a ripple effect on municipal, provincial, and federal levels (World Health Organization, 2021). This conference led to improvements in health policy development, transportation and city planning, medical facility management, fitness centers, and community recreation and park construction even to this day (World Health Organization, 2021). Addressing barriers and understanding health equity has increased public health measures across Canada that has improved the vitality and lifestyle one can achieve in the general population (Doyle & Walker-Baker, 2019).
Operating Principles:
Health equity can be classified as a goal to achieve by all peoples pushing towards a greater space of wellbeing. Health equity also takes into account various components that inhibit or enhance an individual’s ability to live a fulfilling, well-rounded life, such as adaptability or accessibility (Center of Disease Control and Prevention, 2021). These are presented in contrast as health inequities that cause one individual’s accumulation of health equity to differentiate with others around them.
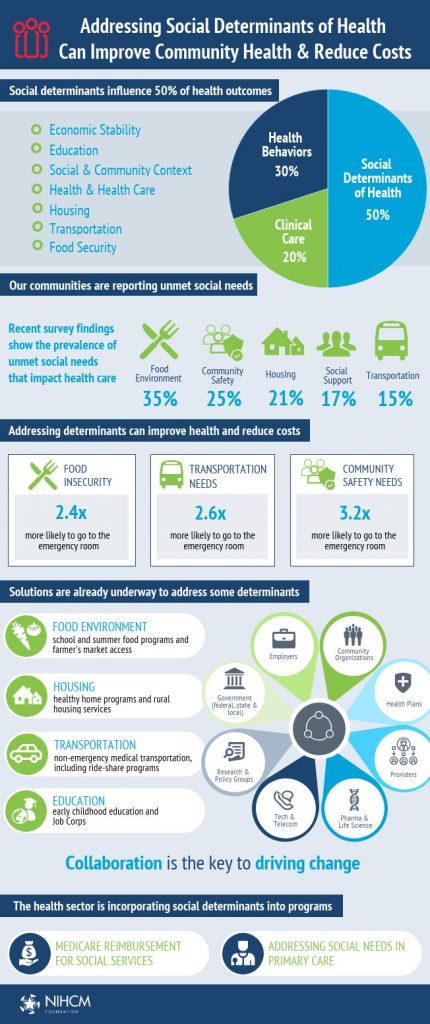
Health equity takes into account several variables that collectively calculate into a comparative value determining one’s holistic wellbeing. These variables often lie outside of the health sector (BC Center for Disease and Control, 2021). These variables include socioeconomic status, financial and emotional wellbeing, education, occupation, disability/ability, and the quality of life of the individual and the environment one resides in. Collectively, an individual’s variables contribute towards one’s ability to obtain health equity.
Figure 2. Infographic illustrating social determinants of health and its intersection in health equity impacting the greater population.
Required Conditions:
Health equity is only achieved if every individual is given the full opportunity to reach their ultimate health potential and no one is disadvantaged due to socially influenced circumstances (Center of Disease Control and Prevention, 2021). Health equity additionally can only be adequately assessed when taking into account the myriad of variables that can challenge an individual’s vitality towards a fulfilling life- and this can differentiate dependent upon the individual and their history.
Negation: Why is health equity important to this day?
Health equity is structurally bound due to health policies, differences in healthcare systems, and financial wellbeing that differentiates across populations. An individual’s ability to achieve health equity can be hindered due to procedures in place such as health insurance (especially in the USA), occupation, and residential location (Fee & Gonzalez, 2021; Doyle & Walker-Baker, 2019). An individual residing in a remote area that requires transportation to centers that have fitness centers, medical facilities, or community centers have lower health equity because the structures in place put them at a disadvantage in terms of accessibility and convenience.
Works cited
BC Centre for Disease Control. (2021). Health equity. Provincial Health Services Authority. Retreived from http://www.bccdc.ca/health-info/prevention-public-health/health-equity.
Center for Disease Control and Prevention. (2020 Mar 11). Health Equity. US Department of Health and Human Services. Retrieved from https://www.cdc.gov/chronicdisease/healthequity/index.html
Fee, E. & Gonzalez, A. R. (2017). The history of health equity: Concept and vision. Diversity and Equality in Health and Care, 14 (3), pp. 148-152. Published by Insight Medical Publishing Group. Retrieved from https://diversityhealthcare.imedpub.com/the-history-of-health-equity-concept-and-vision.pdf
National Institute for Health Care Management. (2020 Oct 21). Addressing social determinants of health can improve community health and reduce costs. NIHCM Foundation. Retrieved from https://nihcm.org/publications/addressing-social-determinants-of-health-can-improve-community-health-reduce-costs
Robert Wood Johnson Foundation. (2021). Visualizing Health Equity: One Size Does Not Fit All Infographic. Achieving Health Equity, An RWJF Collection. Retrieved from https://www.rwjf.org/en/library/infographics/visualizing-health-equity.html#/download
Walker, Ali. & Doyle-Baker, P. (2019 Apr 29). Promoting and strengthening public health through undergraduate education. Canadian Journal of Public Health, 110, pp. 327-330. Retrieved from https://doi.org/10.17269/s41997-019-00217-0
World Health Organization. (2021). WHO called to return to the Declaration of Alma-Ata: international conference on primary health care. World Health Organization. Retrieved from https://www.who.int/teams/social-determinants-of-health/declaration-of-alma-ata.

Leave a Reply