Feasibility Analysis
of a Federal Universal
Dental Program
For
The Honourable Jean Yves-Duclos, Minister of Health
Liberal and NDP coalition for universal dental care
By
Olivia Fournier
English 301 Student
July 22nd, 2022
Table of Contents
Abstract
Introduction
Data Section
Methods of data collection
Demographics of survey participants
Gender
Age
Average yearly household income
Ease of application
Issues reported by participants
Finding an office
Feedback from participants of current programs
Knowledge of program offerings
Lack in coverage reported
Feedback from dental professionals
Issues with current programs
Lack in coverage reported
Switching to a universal dental program
Implementation
Possible issues
Conclusion
Summary of findings
Recommendations
References
Figures and Tables
Table 1
Figure 1
Figure 2
Introduction
Dental care is healthcare; that is a fact. However, even with Canada’s universal health care, millions of Canadians go without recommended preventative and restorative work every year. In fact, only 46% of individuals in a low socioeconomic tier have seen a dentist in the past year (Health at a Glance). This is because in the eyes of the federal government, dental care is seen as a luxury instead of a necessity.
Many publicly funded programs have emerged in the past 15 years; both federally and provincially regulated, in order to help close the gap of lack of care. These programs are targeted primarily to seniors, children, Indigenous populations, and the disabled and have a specific set of qualifiers for eligibility. However, these programs are not limitless and do carry some rules to follow when receiving treatment, and sometimes, what is offered is not enough.
These programs do cover certain procedures and preventative care; however, they have also been the cause of frustration for many patients and dental professionals. As mentioned previously, these programs have limitations, and sometimes the patient requires more aid than what is given. This leads to a gap in healthcare which can be stark. A dental program is not one-size-fits-all and should not be provided as such. Unfortunately, funded coverage is often provided in this way. The 4 programs this report will be analyzing is Health Smiles Ontario (HSO), Ontario Seniors Dental Care Plan (OSDCP), Ontario Disability Support Plan (ODSP), and Non-Insured Health Benefits (First Nations people and Inuit, NIHB) as these are the most common in private practice dentistry.
In early 2022 the Liberal and NDP parties joined forces to begin creating a plan to implement a universal dental care program for those in lower/middle socioeconomic tiers, disabilities, or Indigenous communities. By creating a universal program, it would help to capture more of the population in need and create a standard for those already in the various federal and provincial programs. This analysis will report on the issues participants and dental professionals are experiencing with the current funded dental programs to better formulate a universal care program.
Data Section
Fifty patients from a local private dental practice responded to the survey designed to determine the efficacy and their level of content with their current funded dental program. An analysis was done with these results to evaluate the pros and cons of the current programs in place to determine how a universal dental program would be implemented and run. In addition, interviews were conducted with 4 dental care professionals, 2 dentists and 2 dental hygienists, to examine their views of these programs and what could be made better with a universal system.
Demographics of primary data. Of the 50 individuals who completed the survey, 34 identify as female and 16 identify as male. Median age was 45, with an age range of 5 years old to 78 years old. Household income ranged from $20,000-$80,000 with the average being about $60,000 amongst the participants. Of the 50 participants, 10 were under the age of 18 and parents were asked to fill out the survey in their place. Most participants were a part of the NIHB program for Indigenous people in Canada, with ODSP, HSO, and OCDSP were relatively equal in participation. The participants were asked a series of questions which will be summarized in this analytical report for the readers convenience.
Table 1: Brief survey demographic summary
| Program | Number of survey participants (50) | Female/Male |
| NIHB | 22 | 14/8 |
| ODSP | 10 | 8/2 |
| OSDCP | 9 | 4/5 |
| HSO | 9 | 8/1 |
Ease of application. Out of all the participants, 35 reported that at one point they needed to apply directly for them to be to be covered by a dental program they were eligible for. The other participants either were enrolled directly from birth, such as with NIHB, or by their case manager if they were involved in the social welfare system. Sixty percent of the individuals who needed to apply for the program stated that they had some level of difficulty with the application process. Some common complaints were that the application required documentation the applicant had trouble accessing, or the language used in the application itself was challenging to understand. Upon further research, a report done in 2012 by statistics Canada found that 46% of Canadians in a low-income household had a level 1-2 PIAAC literacy level (Statistics Canada). Therefore, the lower the SES status, the correlation is clear with a lower level of literary and comprehension. The need for auto enrollment or use of plain language is best for a future program.
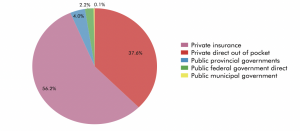
Finding an office. Just over 6% of individual receiving dental care in 2015 were a part of a subsidized dental care program (see Figure 1). Since approximately 73.7% of Ontarians saw a dentist that same year, just under 800,000 Ontarians in a publicly funded program were seeing a dentist in 2015.
Figure 1: Dental Services Expenditures in Canada 2015
In Ontario, many dental offices do not accept patients in funded dental programs. This is another barrier for individuals in these programs, as their local dental office may not accept their method of funding for their important treatments. This is the largest reported problem in the survey. Twenty-three of the fifty participants stated that they had somewhat of a difficult time finding a dental office that would see them while in a dental program. One issue this causes is the influx of patients in offices that do see patients in subsidized dental programs. This leads to the secondary problem of offices that are overbooked and unable to see patients in a timely matter. In a universal system, just like when someone goes to see a doctor, they will not be turned away because of their coverage if the need is present. A law in place to ensure that equity is demonstrated across all patients is crucial moving forwards.
Feedback from participants. Most of the other feedback from participants have been categorized into 2 separate areas of interest.
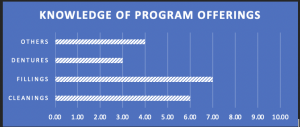
Knowledge of program offerings: Lack of knowledge about what the respective programs cover can result in the participants not taking full advantage of the services available to them Three participants of the survey mentioned that lack of knowledge was a barrier for them, and by looking at the knowledge rating scale, it shows that participants do not have the best understanding of what is available to them. In the survey conducted, participants were asked to rate their knowledge of each section of the program on a scale from 1-10. The highest understanding was for fillings allowance available to them, which is typically 1 filling/tooth/year, which is simple to remember. Cleaning allowances as well as denture programs can be a lot more complicated as the language used is often not in layman’s terms. Training social workers and program coordinators for better patient education is critical for creating better comprehension among participants.
Figure 2: Participants knowledge of their program offerings
Lack in coverage reported: common issues with the current HSO program for children under 18 is that some kids require more than the allotted amount given to them for cleanings. On average a child is seen every 6 months (or 2/year) for a 30–40-minute appointment. While the HSO program does cover this is theory, the amount of time for cleanings can vary drastically per child. For example, one parents reported their child only receiving half of a cleaning while their brother received a full cleaning due to the allowance available.
This is allowance is rarely elongated, and it can be difficult for a dental professional to make a case for the extra time if the child does not have an immediate disability or impairment. This is the case for the other programs as well. The allowance given is often too little for what the patients requires, and unfortunately that treatment or cleaning frequency is not as beneficial as it should be. Some participants reported that they have forgone treatment due to the lack of coverage. Similar to the children’s HSO program, unless extra coverage is requested, which can be difficult to get approved. Dental care is not a one size fits all solution, and it shouldn’t be treated as such. More freedom is required so dental professionals can make the best choice for their patients.
Feedback from dental professionals. As previously mentioned, 2 dentists and 2 dental hygienists from the same clinic offered their anonymous participation as secondary data in this analysis. All dental professional participants are registered with their respective collages and board certified.
Issues with current programs: In the private practice dental office where this secondary information was retrieved, about ¼ or 2,500 patients were a member of a publicly funded dental program. A very high percentage as most offices in the area did not accept dental programs for treatment. While this office had the view that goodwill towards fellow neighbors is best, there are some hesitancies with appreciating the current state completely. One major issue was the lack of fair and proper compensation. The publicly funded dental programs only pay just over half of what the suggested payment for each treatment should be. For example, 30 minutes of cleaning in 2022 in Ontario is $123, the ODSP program will only pay the office $76 for the same 30-minute cleaning.
This has a massive impact on not only the bottom line, but also effects the discrimination greatly. One of the dentists at this office stated that so many people come here because they know we will see them, and often, the staff cannot give them the time they need because they are so overbooked. This was the common sentiment across the clinical staff. All the dental programs in this report do not pay the suggested cost for services. This includes cleanings, fillings, and other work such as crowns and bridges. This is a huge disservice towards participants as it is a huge deterrent for other offices to see them and makes it difficult to see their own dentist due to packed schedules.
Lack of coverage: Like participants, dental professionals also reported a lack of resources for patients. One hygienist stated that to get more time or more cleanings, x rays and a chart of the patient’s periodontal health needs to be sent along to the program office along with their medication list or any health problems they may have. She says that even if there is a great need, unless there is an obvious illness or many medications taken, it will likely be denied, and no further allowance is given. This leaves both the hygienist and patient in limbo where treatment cannot be completed, or they must wait until the next year for their program allowance to reset. It is an endless cycle where eventually an unhealthy mouth can lead to something worse that requires further intervention.
Both dentists interviewed for this report have seen patients put off or forgo very important treatment that has then led to infection or hospital intervention. Research done by Ottawa Public Health showed that between 2004 and 2014, there was a 52-percent increase in visits to emergency rooms for dental related pains and concerns, most of which should been treated in a community setting long before hand (NACRS). By creating a basic and thorough universal program, over-run hospitals stay clean, and patients get help at their first line of defense; their local clinic.
Switching to a universal dental program. In the suggested plan by the NDP and Liberal coalition, the goal would be to supply dental coverage for any families making less than $90,000 annually, additionally, families making under $70,000 per year would not have to pay a deductible or make co-pays for their treatment. Approximately 6.5 million Canadians would be eligible for this program, including those currently under the care of a subsidized dental program. The plan is going to be implemented in the next 3 years with children under 12 being covered by the end of 2022, and individuals with disabilities, seniors, and people under 18 being covered by the end of 2023. This program is projected to cost over 4 billion dollars in the first year, due to existing treatment that Canadians will finally be able to access, and afterwards should cost about 1.5 billion dollars a year. Due to the higher volume of services needed, and the current lack of dental offices who accept payment from publicly funded dental care, there would need to be regulation in place to ensure that proper payment is provided for services determined by the Canadian Dental Association. This will ensure that offices are compensated fairly and individuals under a universal program would be treated with dignity and respect.
Possible issues: dental professionals reported some hesitation with introducing a universal program. The challenge with introducing large groups of people at once could cause some traffic in the private sector due to difficult and medically complex cases to treat. This is where public health services would be of utmost importance. I envision a way for public health dental professionals to help and treat these individuals, as well as help to prioritize cases in order of importance and impact on patients’ wellbeing. This triage would help to find offices for patients depending on their location to help with patient coordination and bookings. Issues along the way are a part of any new program implementation, having the supportive infrastructure underneath is the best step forwards.
Conclusion
This analytical report ties together primary and secondary data from multiple sources. Participants of these programs, being the primary data source and producing incredible feedback that would lead to a better conducted universal dental care program. Dental professionals are a crucial secondary source for looking at how this effects the dental profession, as well as feedback on how to make the program more effective for patients from a provider’s point of view. A federal universal dental program would benefit from this report and from the proposed solution. To review, there are 4 main areas of concern when shaping a new program.
- Lack of coverage
- Finding an office
- Language/literacy barriers
- Insufficient payment for offices
In order to solve these issues, there are some recommended changes needed for a universal dental program. I will briefly go over the recommended changes for each issue addressed.
Lack of coverage: in a universal system, 8 units of time for cleanings should be provided for anyone over 18, and 4 units for under 18-year old’s, with an easier was to ask for additional units of time that can be explained using x rays or plaque indexes instead of needing there to be a disability or multiple medications as reasons. In terms of restorative work, one tooth can be worked on per year, however there should be a way to provide emergency assistance should someone need something done immediately, or a way to co-pay it if the treatment is more complicated.
Finding and office: in terms of finding a dentist and an office to seek treatment, the universal program should follow in the path of Medicare care and make it so a patient cannot be turned down because of their coverage. Ending healthcare discrimination would be the goal. Furthermore, it is my recommendation that public health dental professionals work in a triage/coordination role to help individuals who do not currently have a dentist set up with an office that works for them. This should help to minimize the long wait times, and to prioritize those with difficult or painful issues that are ongoing.
Language and literacy barriers: the medical field has always been difficult for anyone of all literacy levels and education to navigate. A common issue among participants was that the application process was difficult to complete at times due to misunderstanding information. Bringing in a language pathologist and looking into easier ways of wording these applications would help drastically. Another recommendation would be public health administrators would be tasked to help fill out these forms or request information on behalf of the patient to help them with enrollment. By making the federal universal program straightforward and comprehensible there will be a greater chance of uptake with the public.
Payment for offices: while not a significant barrier to proper treatment, the fact that the current programs only pay just over half to ¾ of current treatment costs are significant when running a dental clinic. It creates underlying discrimination, and that is unfair to program participants. In a universal program, treatments costs should be following the Canadian Dental Associations fee guideline to ensure patients are treated with dignity and with time a time efficient manner. These patients should not be seen as lesser than those who can afford to pay full price or who have private insurance coverage. At its core, healthcare needs to be accessible and attainable for all.
By following these recommendations brought forth by issues from primary and secondary data evaluating these publicly funded dental care programs, a better and more comprehensive federal universal dental plan can be created. At the core of this report were the participants who graciously submitted survey responses and provided feedback for what was lacking in their care. Dental is healthcare; and that statement should drive the success of this universal program moving forwards.
References
Canadian Institute for Health Information. National Health Expenditure Trends, 1975 to 2015. Ottawa: CIHI; 2015. Available: https://www.cihi.ca/sites/default/files/document/ nhex_trends_narrative_report_2015_en.pdf
National Ambulatory Care Reporting System (NACRS), Ontario Ministry of Health and Long-Term Care, IntelliHEALTH ONTARIO, Date Extracted: Sept 2018.
OECD (2011). Health at a Glance 2011: OECD Indicators. France: OECD Publishing; 2011. Available: http://www. oecd.org/els/health-systems/49105858.pdf
Statistics Canada, Longitudinal and International Study of Adults (LISA), 2012. Available: https://www150.statcan.gc.ca/n1/pub/75-006-x/2016001/article/14322-eng.htm
Dental care programs Ontario ( word doc)
Leave a Reply