Integration of Traditional Indigenous Medicine in Contemporary Indigenous Communities
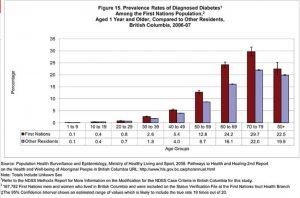
Diseases and conditions, such as diabetes, HIV/AIDS and mental illness, are at a higher prevalence within Indigenous communities compared to non-Indigenous communities. The implementation of western health care prevention and treatment strategies are seemingly not effective enough to combat these alarming statistics. I am exploring the reasons why these interventions are not effective by looking at the transgenerational impacts that are still lingering from enforced attendance in Residential Schools as well as the systemic racism that prevents Indigenous peoples from seeking healthcare.
PEER-REVIEWED ARTICLES
1) Bagelman, J., Devereaux, F., Hartley, R (2016). Feasting for Change: Reconnecting with Food, Place & Culture. International Journal of Indigenous Health, 11(1). Doi: 10.18357/ijih11201616016
- Speaks about the decolonization of western health practices and discourses in Indigenous communities through a project called, “Feasting for Change”.
- The goal of the project is to empower Indigenous communities, to revitalize traditional knowledge, and to discuss the healing powers of food
2) Eid, H.M, Haddad, P.S. (2014). Mechanisms of Action of Indigenous Antidiabetic Plants from the Boreal Forest of Northeastern Canada. Advances in Endocrinology 2014. Doi:10.1155/2014/272968
- Exploring the efficacy of traditional medicinal plants from Indigenous Traditional Medicine in the Boreal forest in the treatment of Type 2 Diabetes.
- Provides an interesting avenue for traditional Indigenous medicine to be introduced into mainstream health care as a treatment for Type 2 Diabetes, rather than western medicine being imposed into Indigenous communities
3) Ghosh, H., Gomes, J. (2011). Type 2 Diabetes among Aboriginal Peoples in Canada: A Focus on Direct and Associated Risk Factors. Pimatisiwin: A Journal of Aboriginal and Indigenous Community Health 9(2).
- Acknowledges that thus far, diabetes intervention strategies have not been successful because it has not offered Aboriginal-specific prevention strategies
- This paper looks at the multifaceted risk factors for diabetes (modifiable, intermediate, and nonmodifiable) in order to develop specific interventions
4) Goodman, A., Flemin, K., Markwick, N., Morrison, T., Lagimodiere, L., Kerr, T. (2017). “They treated me like crap and I know it was because I was Native”: The healthcare experiences of Aboriginal peoples living in Vancouver’s inner city. Social Science & Medicine 178, 87-94. Doi:10.1016/j.socscimed.2017.01.053
- A study of the experiences of Aboriginal peoples who use illicit drugs or alcohol and live in Vancouver’s inner city
- This study was done using Indigenous methodologies, straying away from colonialist approaches
- Demonstrates that systemic racism is still very much present and affects the healthcare that Aboriginals people receive
5) Hackett, C., Feeny, D., Tompa, E. (2016). Canada’s residential school system: measuring the intergenerational impact of familial attendance on health and mental health outcomes. Journal of Epidemiology and Public Health, 70, 1096-1105. Doi: 10.1136/jech-2016-207380
- This statistical study looks at the long term effects of residential schools on Indigenous families by looking at the intergenerational prevalence of different mental health disorders
- Shows that familial residential schools definitely had an impact on mental health issues in these families
6) Howell, T., Auger, M., Gomes, T., Brown, F.L., Leon, A.Y. (2016). Sharing Our Wisdom: A Holistic Aboriginal Health Initiative. International Journal of Indigenous Health, 11(1). Doi: 10.18357/ijih111201616015
- This paper focuses on understanding and describing Aboriginal traditional healing methods in place or as an adjuvant to mainstream health practices
- The paper also stays away from traditional research practices and instead incorporates traditional Aboriginal knowledge sharing which helped to foster participation
7) Jacklin, K.M., Henderson, R.I., Green, M.E., Walker, L.M., Calam, B., Crowshoe, L.J. (2017). Health care experiences of Indigenous people living with type 2 diabetes in Canada. CMAJ 189(3). Doi:10.1503/cmaj.161098
- To study how colonization has impacted Indigenous health
- The experiences of Indigenous peoples in regards to health care
8) Laurie Meijer Drees (??). Reserve Hospitals and Medical Officers: Health Care and Indian Peoples in Southern Alberta, 1890s-1930.
9) MacDonald, C., Steenbeek, A. (2015). The Impact of Colonization and Western Assimilation on Health and Wellbeing of Canadian Aboriginal People. International Journal of Regional and Local History 10(1). Doi:10.1179/2051453015Z.00000000023.
- This research article adapts a post-colonial, feminist, theoretical approach to begin to understand the inequalities that Aboriginal peoples face in health.
- The researchers focus on how colonization and the subsequent assimilation of Aboriginal people
- Health problems are looked at in multifaceted contexts such as historical, economic, and socio-political
10) Marielle Christine Leilani Young (2016). To Empower and Educate: Bringing Native Students into the Healthcare Professions. Tribal College Journal, 27(4), 46-47.
- http://web.b.ebscohost.com/ehost/detail/detail?sid=6debc74c-b0bc-4c80-bb84-18a1eb4ab7a1%40sessionmgr101&vid=0&hid=123&bdata=JnNpdGU9ZWhvc3QtbGl2ZSZzY29wZT1zaXRl#db=fph&AN=115246639
- This article describes efforts to engage with Indigenous college students to speak about the health issues that are prevalent in Indigenous communities
- The goal of engagement is to peak these students’ interests in health care and its applicability to their tribes in order to bring them into healthcare professions
11) Rice, K., Te Hiwi, B., Zwarenstein, M., Lavallee, B., Edward, D., Harris, S.B. (2016). Best Practices for the Prevention and Management of Diabetes and Obesity-Related Chronic Disease among Indigenous Peoples in Canada: A Review. Canadian Journal of Diabetes, 40(3). 216-225. Doi: http://dx.doi.org/10.1016/j.jcjd.2015.10.007
- A colonialist approach to providing intervention programs, such as dietary changes or exercise changes, to better manage diabetes in Indigenous communities
- They claimed to doing little to address the systemic marginalization and colonialization experiences in these communities, and it is interested to note that the intervention programs did very little in managing diabetes
12) Sheehy, T., Kolahdooz, Schaefer, S.E., Douglas, D.N., Corriveau, A., Sharma, S. (2014). Traditional food patterns are associated with better diet quality and improved dietary adequacy in Aboriginal peoples in the Northwest Territories, Canada. Journal of Human Nutrition and Dietetics, 28(3), 261-271. Doi:10.1111/jhn.12243.
- With colonization came import of processed foods that do not agree with Aboriginal peoples adaptations to their traditional diets
- Researchers looked at the nutrients in traditional and non-traditional diets, as well as traditional and non-traditional peoples, and found that Aboriginal peoples who ate traditional foods had better quality of diet.
- Return to traditional diets could help with intervention of obesity-related diseases, such as diabetes
13) Tang, T., Community Wellness Program, Jardine, C.G. (2016). Our Way of Life: Importance of Indigenous Culture and Tradition to Physical Activity Practices. International Journal of Indigenous Health 11(1). Doi: 10.18357/ijih111201616018
- Inactivity is a leading cause of type 2 diabetes. This article looks at how Indigenous youth are developing videos to encourage physical activity, while integrated culture, tradition, participation, and theme of culture identity
- This article demonstrates the ways that Indigenous youth are taking part of acts of decolonization to promote their own culture while creating preemptive measures against disease
BOOKS
14) Allan, B, Smylie, J. (2015). First Peoples, Second Class Treatment: the Role of Racism in the Health and Well-Being of Indigenous Peoples in Canada. Canada, Toronto, ON: the Wellesley Institute.
- How the health of Canada’s Indigenous peoples have been impacted by racism and colonization
- Speaks about the experiences of Indigenous peoples in regards to health care and well-being from an Indigenous perspective
- Discusses the barriers that Indigenous peoples face when trying to access healthcare
15) Vasiliki Douglas (2013). Aboriginal Health and Health Care in Canada: Bridging Health and Healing. New York NY: Springer Publishing Company.
This book goes in depth about the issues prevalent in First Nations, Metis, and Inuit communities in Canada, the differences between western and Aboriginal ways of knowing, and the different health problems that are prevalent within these communities
NEWSPAPER ARTICLES
16) Hoath, L., Sturino, I. (2016 Jun 21). Meet Dr. Nadine Caron, Canada’s first female First Nations. CBC Radio. Retrieved from:http://www.cbc.ca/radio/thecurrent/the-current-for-june-21-2016-1.3644974/meet-dr-nadine-caron-canada-s-first-female-first-nations-surgeon-1.3645029
- An article written about Dr. Caron, who is Canada’s first female First Nations surgeon
- Writes about the existing racism towards First Nations patients and even towards herself, and the problems that colonialism still perpetuate in today’s society
17) Lefebvre, D. (2013 Jun 21). Traditional Aboriginal Medicines Find a Home at St. Paul’s Hospital. Providence Health Care. Retrieved from http://www.providencehealthcare.org/news/20130625/traditional-aboriginal-medicines-find-home-st-pauls-hospital
- Paul’s Hospital in Vancouver, BC opened an All Nations Sacred Space
- “Provides an area for smudging and pipe ceremonies, recognizing these traditional medicines as an important component of aboriginal health care”
- “By bringing traditional aboriginal medicines into our hospital, we’re opening our doors to the aboriginal community and expressing our desire to accommodate their culture”
18) McCue, D. (2015 Feb 03). Racism against aboriginal people in health-care system ‘pervasive’: study. CBC News. Retrieved from: http://www.cbc.ca/news/indigenous/racism-against-aboriginal-people-in-health-care-system-pervasive-study-1.2942644
- This short clip shows interviews about Aboriginal people who have faced discriminatory profiling when seeking medical treatment in hospitals.
- Also brings up integration of traditional aboriginal healing techniques in mainstream, colonial hospitals
19) Morris, N. (2016 Feb 28). Residential Schools in Canada, and Why It Matters in Health. Canadian Foundation for Healthcare Improvement. Retrieved from: http://www.cfhi-fcass.ca/SearchResultsNews/2016/02/26/residential-schools-in-canada-and-why-they-matter-in-health
- This information page gives a short and sweet summary on why people need to consider the history of residential schools and why it affects the health of Indigenous peoples
SHORT CLIPS
20) Tremonti, A.M. (2013 Jan 30). State of Care Documentary: Canada’s segregated health care. CBC Player. Retrieved from: http://www.cbc.ca/player/play/2330496879
- This piece explores the emergence and establishment of ‘Indian-only hospitals’ that allowed segregation of Indigenous patients from white patients
- Indian-only hospitals were first established to treat tuberculosis, which was prominent during the residential school era, but soon began to treat not only TB, but also served to be a general hospital