I am tuning in from winter in Cambodia (there was a cold-weather advisory recently… this afternoon it got up to 29 degrees). Thank you for your patience in the LONG silence between posts.
I am more than overdue to provide you with an overview of the nutrition research that my university is conducting in collaboration with a local NGO in Phnom Penh that I have the privilege to be a part of. AKA we are answering the “what are you researching?” question. We are about to get real science-y but I promise you I’ll really break it down. Stick with me…
Let’s start off with some background and definitions.
Anemia -What is it? Hint: it’s not “iron deficiency”. Well, at least not simply that.
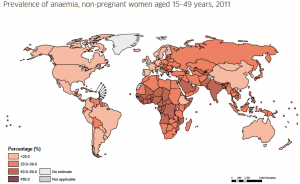
Anemia is a huge problem worldwide, affecting over 1.5 billion people (yes, you read that right). Anemia is when you have low red blood cells, meaning not enough oxygen is circulating around your body reaching vital tissues, causing fatigue, decreased work productivity, and adverse pregnancy outcomes, just to name a few of its detrimental consequences.
Oftentimes, people think iron deficiency is synonymous with anemia, but this is not true and it is important to understand the difference.
Hemoglobin is a protein in your red blood cells that binds iron, making iron an essential element for red blood cell production. Iron deficiency has 3 stages. In the most severe stage, when iron stores are exhausted, there is inadequate iron for sufficient red blood cell production. This refers to iron deficiency anemia and is generally assumed to cause about half of all anemia cases worldwide. But many other things can also cause anemia: other micronutrient deficiencies (folate, vitamin B12), excessive blood loss through heavy menstruation, inflammation, infection (eg malaria), or genetically inherited disorders affecting hemoglobin production (aka genetic hemoglobin disorders).
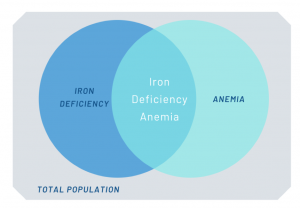
Global recommendations state women of reproductive age should consume 60mg iron supplements daily for 3 consecutive months each year in countries where anemia prevalence is greater than 40%, including Cambodia (with 45% of women having anemia in 2014!!!). This recommendation is based on the assumption that ~50% of anemia in low-income countries is caused by iron deficiency (ID), along with the well-established benefit of iron supplementation to correct ID. It is important to note that iron deficiency is only one (of the many) causes of anemia and giving iron to anemic women will only be helpful if iron deficiency is the cause of their anemia.
It has generally been assumed that, in Cambodia, the majority of anemia is associated with insufficient iron intake. The country has adopted many iron supplementation programs, such as iron and folic acid pills for pregnant- women, iron in birth control pills, and fortifying fish sauce country-wide with iron, but rates of anemia have not changed over the years. In recent studies, they found a low prevalence of iron deficiency – only ~3% of Cambodian women had ID. So, if iron deficiency is not the major cause of anemia in a population, untargeted iron supplementation and is a waste of resources; and at worst, it could cause harm.
Anemia in Cambodia is largely associated with genetic hemoglobin disorders (60% of women have these disorders!!), making the potential for iron supplementation to cause harm especially true, as these disorders cause altered iron metabolism and an increased risk of iron overload.
Given global policies and implementation programs, it is necessary to understand the potential harms of supplementation. Countless studies have reported on the benefits of iron supplementation and fortification but there is a huge lack of research looking at harm, beyond gastrointestinal upsets (if you’ve taken iron pills before you may know you can get stomach aches or other GI symptoms). Excess iron is known to be associated with many consequences, including oxidative stress, DNA damage, gut pathogen abundance and gut inflammation. When you have excess iron siting unabsorbed in your colon it feeds pathogenic bacteria, overriding beneficial bacteria, throwing off the equilibrium of the gut microbiota, resulting in increased inflammation within your gut.
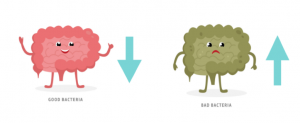
The risks are made greater because the type of iron that is commonly used in large-scale programs is poorly absorbed. Typically, less than 20% is absorbed in the gut; the remaining 80% passes unabsorbed in the colon, where it can increase that risk of pathogen growth and gut inflammation. But what if a higher bioavailable form of iron was given? This way a much lower (and potentially safer) dose would be necessary.
If you are still reading WELL DONE! I appreciate your curiosity!
So after that long background…. our study is seeking to understand the safety of blanket iron supplementation in anemic populations where iron deficiency is not the main cause of anemia and hemoglobin disorders are common.
We are comparing a newer type of iron that is much better absorbed (giving a much lower dose) to the conventional form and dose or iron recommended worldwide. This novel iron is very common in Canada, USA and Europe. We are comparing how these forms impact iron levels in the body as well as markers of potential harm in the gut, DNA and more.
We are recruiting women from a rural province 3 hours away from the capital city of Phnom Penh. Participants will be randomly assigned to one of the three treatment arms, and receive supplement bottles with instruction to take a pill every day (either (1) conventional iron, (2) high bioavailable iron or (3) placebo [control group]).
I am working with a fantastic team as we move through the many stages of the study: recruitment, enrollment, questionnaires, blood and stool collection time points and continual monitoring visits over 4-5 months.

The hope of this study is that it will contribute to the evidence for safe and effective iron supplementation for women in Cambodia and worldwide.
I will post day-in-the-life field updates along the way with lots of photos because I know that this will be the more exciting part to read about! Stay tuned. I pinky promise I won’t take months before my next update.

Thank you Jordie!!
Thanks for the update Jordie. So informative!