PCK/TPACK were definitely new terms for me. Though my idea of a “good” teacher was one who had both content knowledge and pedagogical knowledge specific to that content, I had never heard of it being described in such a concise manner. Looking at the many physicians that teach, particularly at the clinical level, they are definitely content experts with little or no pedagogical knowledge. Somehow it is presumed that having the content knowledge gives you the ability to teach medicine, which is far from the truth, and I have personally been on the receiving end of this. For example, experienced physicians are able to accomplish tasks in an “unconscious competent” manner. Looking at the diagram below, novice students and residents start at the “unconscious incompetent” stage of this cycle.
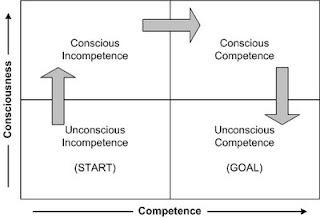
They observe an expert accomplish something (such as suturing) and because the expert made it look so easy, presume that it can easily be accomplished. When they are given the opportunity to do the task themselves, they move into the “conscious incompetent” stage, where they begin to understand that it isn’t as easy as it looks and there are a lot of steps that they had not considered upon observation. With repeat practice, reflection, and learning with guidance, they enter the “conscious competent” stage, where they still have to think about each step but can complete the task competently. Clinical teachers facilitate their learners through this cycle, but because many of them are doing tasks in the “unconscious competent” state, sometimes they are unable to identify some of the steps that are automatic for them, and thus are missing the pedagogical knowledge component.
A common procedure that I perform that is difficult to learn is insertion of a device called a TVT. This device is used for the treatment of stress incontinence. It is difficult to learn because it is a relatively blind procedure, with a high bladder injury rate (which increases learner anxiety!) When teaching this procedure, I often break it down into several steps for my residents:
1) Observation – I will have them observe the procedure as I perform it. I will deliberately take my time performing each step, and explain each step as well as the rationale behind my movements.
2) Then I take them over to a pelvic model for simulation (after the observation). Again, I repeat the procedure, performing each step slowly and with explanation. I will also have them slide their hands over mine to feel where I am in relation to the anatomy (because most of it is done blindly).
3) Next, I have the learner verbally repeat the steps while visualizing
4) Then I have them perform the steps, verbalizing each step as perform it (on the model simulator).
5) I will have them repeat this on the model a few times until they are comfortable
6) At the next OR, if this procedure comes up, I will have them verbalized the steps with visualization prior to the case.
7) Finally, I will have them perform the case, while verbalizing each step, and provide guidance as needed. At this point, I gauge their level of comfort and competence and adjust my guidance as needed.
Over the last couple of years that I have been teaching this, I have modified the steps based on the areas that my learners seem to struggle the most. These areas are broken down into smaller steps, with simple instructions so the procedure is easier to understand and perform.
