I decided to summarize the 4 TELEs in table format. This is what I came up with:
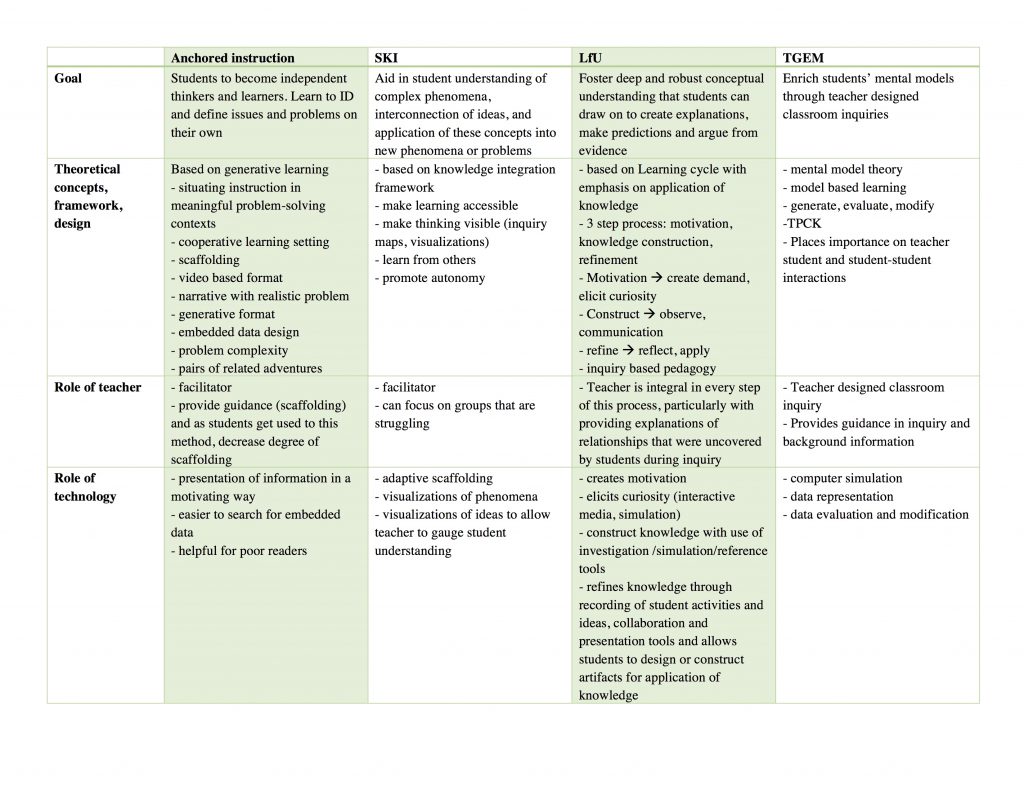
Below is a link to a PDF in case the above does not read well.
Module B synthesis
My personal journey through ETEC 533
I decided to summarize the 4 TELEs in table format. This is what I came up with:
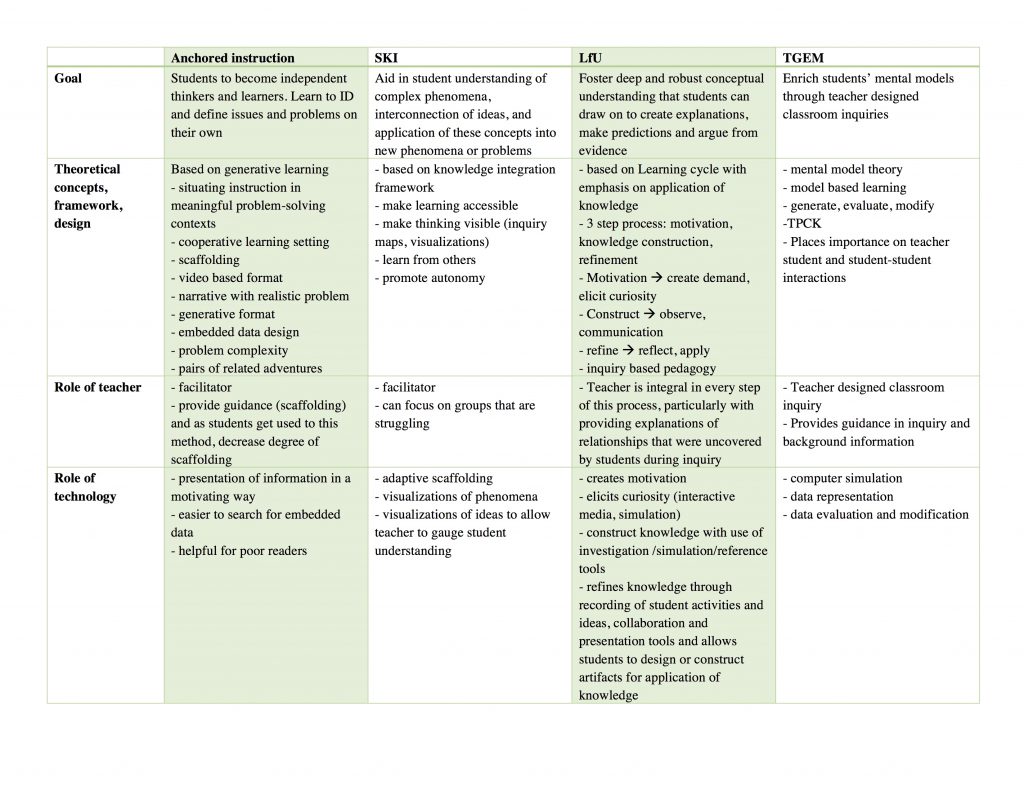
Below is a link to a PDF in case the above does not read well.
Module B synthesis
A commonly cited conceptual challenge in medical education is cardiovascular physiology. This seems to be a consistent finding at different educational levels (Mikkila-Erdmann, 2012). If applying the T-GEM model (Khan, 2010)to teaching this, I would organize it as follows:
I think this method will offer students a chance to challenge their conceptual models by simulation and make modifications as needed. In trying to find software for TGEM in the medical context, I ran into a significant challenge. This is because a lot of medical simulations were for clinical skills or other technical skills improvement, and not for the purposes of understanding certain phenomena. But I do think this is a great way to learn and really understand concepts in a deeper more meaningful way (compared to the superficial rote memorization that is still common in medical education). I hope that simulations that examine concepts in my field become more readily available as time goes on.
References
Khan S. New Pedagogies on Teaching Science with Computer Simulations. J Sci Educ Technol. 2010;20(3):215-232. doi:10.1007/s10956-010-9247-2.
Mikkilä-Erdmann M, Södervik I, Vilppu H, Kääpä P, Olkinuora E. First-year medical students’ conceptual understanding of and resistance to conceptual change concerning the central cardiovascular system. Instr Sci. 2012;40(5):745-754. doi:10.1007/s11251-012-9212-y.
According to Edelson (2001), LfU is based on 4 theories of learning, which are:
1) learning takes place through construction and modification of knowledge structures
2) knowledge construction is a goal-directed process, guided by a combination of conscious and unconscious understanding of goals
3) circumstances in which knowledge is constructed and subsequently used determine its accessibility for future use
4) knowledge must be constructed in a form that supports use before it is applied.
These principles underlie the LfU model, which is a three-step process involving
1) motivation
2) knowledge construction
3) knowledge refinement
In terms of technology, it plays many important roles within the LfU model. For example, it can play a role in eliciting curiosity (motivation), help students interactive with phenomena not possible in the real world which aids with knowledge construction and refinement.
So how would I apply it to a topic that I teach? The one thing that comes to mind is pelvic anatomy. Students tend to struggle with pelvic anatomy because it is quite complex and has multiple layers to it. I would start off by presenting students with a case of a patient who underwent surgery and shortly thereafter developed leg weakness and pain (this is actually one of the patient that presented to me early in my career). I would then have the students come up with theories based on their current knowledge level, regarding the cause of this pain/leg weakness. This is to draw their attention to their current level of knowledge and to have them recognize their limitations and thus increase motivation to learn. This would also create a context in their memory for integrating new knowledge (Edelson, 2001). Then I would use AnatomyTV, which is an interactive 3D anatomy resource (available through UBC at http://resources.library.ubc.ca/page.php?id=888) as my software of choice. This interactive resource that allows students to manipulate the body in 3D (select 3D Atlas —> Pelvis, then click female pelvis and perineum ~ tumble under 3D views from menu on the left to try it out!), which is really helpful, as most textbooks only present the learner with the upright position of the human body. This is not practical because in most gynecologic clinical practices, we examine patients and operate on them in the supine position, and thus knowledge of anatomy in this position is much more applicable. This program also allows the user to strip away all layers of the body and add them one by one, which allows students to understand how each layer relates to the other. I would also have student work in small group to promote interaction and discussion as this also aids in knowledge construction and refinement. Finally, I would have the students reflect on their initial theories, make any changes they feel are needed and present it as a group to the class and further apply their new knowledge to come up with a management plan for the patient. In this way, I believe I have applied the LfU principles to this topic.
References
1. Edelson DC. Learning‐for‐use: A framework for the design of technology‐supported inquiry activities. Journal of Research in Science Teaching. 2001;38(3):355-385. doi:10.1002/1098-2736
This week, I read a lot about WISE (Web-based Inquiry Science Environment) projects. The project’s creation was motivated by a state and national call for inquiry learning, which the creators found was minimal in the science class room. WISE is based on a knowledge integration framework. Their research indicated that students try to make sense of complex phenomena, but were unable to interconnect these ideas or apply them to new problems or phenomena (Slotta & Linn, 2009). The knowledge integration framework emerged to make sense of ideas that students bring to class with them, make learning of science more efficient (through an inquiry method), and help connect existing ideas with new ideas.
According to Linn, Clark and Slotta (2003), there are 4 tenants of knowledge integration framework:
Each WISE project is created with these tenants in mind. It also follows a general instructional pattern as follows:
So far in this course, we have been introduced to the Jasper series as well as WISE projects. I believe the main difference between the two is the degree of guidance or scaffolding that is provided. In the Jasper series, a more generative process is desired. Whereas the WISE projects have inquiry maps which provide students with a guide during their inquiry process. I think both approaches are valuable, and one will appeal to some students more than others, and this distinction is based on personal preference, degree of autonomy and level of knowledge. Both strategies are highly adaptable, and the Jasper series could be used in a more guided process, just as the WISE projects can be adapted to provided less guidance.
In terms of how I would use wise, I think it is very similar to case based learning at our institution. I think I would be able to create a WISE project using some of the case based learning integrated with some lecture material to provide normative information. The customization I would perform is only to the inquiry map. As mentioned by Linn, Clark and Slotta (2003), if the inquiry steps are too precise, students fail to engage, but if too broad, students may be easily distracted and not motivated to complete the project. Based on the type of learners I have, I think I can make the inquiry steps a little broader.
References
Linn MC, Clark D, Slotta JD. WISE design for knowledge integration. Science Education. 2003;87(4):517-538. doi:10.1002/sce.10086.
Slotta JD, Linn MC. WISE Science: Inquiry and the Internet in the Science Classroom. Teachers College Press. 2009.
The theoretical framework that underpins the Jasper series is anchored instruction. Anchored instruction is instruction that is “situated in engaging, problem-rich environments that allow sustained exploration by students and teachers” (Cognition and Technology Group at Vanderbilt, 1992). The Jasper series is a video based instruction format that presents students with a complex problem, which requires many subproblems to be generated and solved for the main complex problem to be addressed. It uses an engaging narrative with embedded data to present the students with all the information they may require to engage with the complex problem. This instructional approach promotes several teaching and learning activities that are central to constructivism. This includes generative learning, collaboration, active learning and engagement, and construction of knowledge.
Certainly the Jasper series could be presented without the use of technology. However technology does enhance the teaching and learning activities mentioned above. For example, the use of video could make the material more engaging due to the increased realism afforded by the video format (though it is a little dated now). This notion is supported by several papers, as highlighted by Taylor and Parsons (2011) in their review of the literature on student engagement. It can also be helpful for those students with learning challenges where an audio only narrative or reading only narrative would present a significant barrier.
Medical education has certainly moved in this direction. During the first two years, we have increased exposure of students to real clinical environments where they would learn though clinical encounters in a situated learning environment. In addition to this, their didactic lectures are taught along side problem-based learning activities, which is essentially anchored instruction. Our school currently does not use a video format, but a written digital document is provided to students in small groups, which gives students a clinical scenario. They then discuss the case to figure out what is going on with the patient. In all groups, the members decide on what further knowledge is needed in order to move forward with the case scenario. During this discussion portion, they are not allowed to use any resources other than their own ideas and experiences, which promotes discussion, collaboration and reflection. Once they have established learning objectives for the group, the first session ends and they have 1-2 days to research their learning objectives (either collaboratively or individually, depending on the group). They then reconvene and discuss the learning objectives before more of the clinical scenario is revealed. Typically, each case is discussed over 2-3 group sessions.
I think that in our problem-based learning groups, technology can be used to enhance collaboration and generative learning. For example, concepts maps may be useful to organize the group’s thoughts in a visual manner, adding to collaboration and generation of ideas. The use of something like Google Docs which affords collaboration asynchronously could also be helpful in collaboration outside of the group meetings. A video format could also be helpful to refine students’ observational skills as this is a critical part of the medical assessment, and again help to create an authentic/realistic environment.
References
Cognition, Vanderbilt TGA. The Jasper experiment: An exploration of issues in learning and instructional design. ETR&D. 1992;40(1):65-80. doi:10.1007/BF02296707.
Taylor, L. & Parsons, J. (2011). Improving Student Engagement. Current Issues in Education,14(1). Retrieved from http://cie.asu.edu/
PCK/TPACK were definitely new terms for me. Though my idea of a “good” teacher was one who had both content knowledge and pedagogical knowledge specific to that content, I had never heard of it being described in such a concise manner. Looking at the many physicians that teach, particularly at the clinical level, they are definitely content experts with little or no pedagogical knowledge. Somehow it is presumed that having the content knowledge gives you the ability to teach medicine, which is far from the truth, and I have personally been on the receiving end of this. For example, experienced physicians are able to accomplish tasks in an “unconscious competent” manner. Looking at the diagram below, novice students and residents start at the “unconscious incompetent” stage of this cycle.
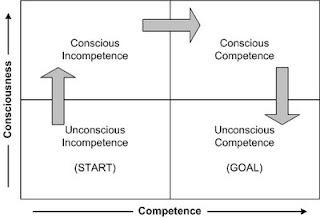
They observe an expert accomplish something (such as suturing) and because the expert made it look so easy, presume that it can easily be accomplished. When they are given the opportunity to do the task themselves, they move into the “conscious incompetent” stage, where they begin to understand that it isn’t as easy as it looks and there are a lot of steps that they had not considered upon observation. With repeat practice, reflection, and learning with guidance, they enter the “conscious competent” stage, where they still have to think about each step but can complete the task competently. Clinical teachers facilitate their learners through this cycle, but because many of them are doing tasks in the “unconscious competent” state, sometimes they are unable to identify some of the steps that are automatic for them, and thus are missing the pedagogical knowledge component.
A common procedure that I perform that is difficult to learn is insertion of a device called a TVT. This device is used for the treatment of stress incontinence. It is difficult to learn because it is a relatively blind procedure, with a high bladder injury rate (which increases learner anxiety!) When teaching this procedure, I often break it down into several steps for my residents:
1) Observation – I will have them observe the procedure as I perform it. I will deliberately take my time performing each step, and explain each step as well as the rationale behind my movements.
2) Then I take them over to a pelvic model for simulation (after the observation). Again, I repeat the procedure, performing each step slowly and with explanation. I will also have them slide their hands over mine to feel where I am in relation to the anatomy (because most of it is done blindly).
3) Next, I have the learner verbally repeat the steps while visualizing
4) Then I have them perform the steps, verbalizing each step as perform it (on the model simulator).
5) I will have them repeat this on the model a few times until they are comfortable
6) At the next OR, if this procedure comes up, I will have them verbalized the steps with visualization prior to the case.
7) Finally, I will have them perform the case, while verbalizing each step, and provide guidance as needed. At this point, I gauge their level of comfort and competence and adjust my guidance as needed.
Over the last couple of years that I have been teaching this, I have modified the steps based on the areas that my learners seem to struggle the most. These areas are broken down into smaller steps, with simple instructions so the procedure is easier to understand and perform.
When I first started in my ETEC journey, my definition of technology was very general. Just as Muffoletto (1994) describes, I thought of it “in terms of gadgets, instruments, machines, and devices” that assist humans in achieving a task. But as I journey through this program, my ideas of technology started to change, particularly in regards to educational technologies. As such, the definition by Jonassen (2000) really resonates with me. I feel in order for something to be considered an educational technology it should have the features of what Jonassen (2000) terms “mind tools”; those tools which help construct knowledge, not just disseminate information to the learner. This leads to a deeper understanding of information and internalization/reorganization within the learner.
In regards to design of my ideal TELE in med ed, it would be a small room that looks like of the picture below from minority report (TV show).
 Minority Report
Minority Report
A group of 5-8 students, would work around together around technology enhanced table to do problem based learning. The technology would be used to organize their collaborative thoughts, collect data, communicate ideas between members, and manipulate certain parameters (if appropriate) in order to progress through a medical problem. I think educational technology should be a tool that helps construct knowledge, and the environment should allow for collaboration and team work.