In the last 10 years in Canada, care providers, health authorities and governments have been working hard at developing and implementing electronic health systems. In this post, I explore these new technologies, and Electronic Medical Records (EMR) in particular. What are the benefits and challenges of these systems? What are the guidelines around consent and privacy for health authorities and Social Workers.
UBC School of Social Work: Prezi Presentation
Notes from my presentation at the School of Social Work at UBC, September 2018.
Our goals:
- Increase our interest and knowledge of new technologies being implemented by health authorities
- Understand possible benefits and challenges of these new technologies
Improve our understanding of Social Work practice in the context of new technologies
Main topics:
1- New Technologies and EMR
2- Consent and Privacy
3- Social Work Practice and EMR
What are these electronic systems? EHR vs EMR?
Electronic Health Records (EHR): “a complete health record under the custodianship of a health care provider(s) that holds all relevant health information about a person over their lifetime. This is often described as a person-centric health record, which can be used by many approved health care providers or health care organizations.” (www.infoway-inforoute.ca).
Electronic Medical Records (EMR): “a partial health record under the custodianship of a health care provider(s) that holds a portion of the relevant health information about a person over their lifetime. This is often described as a provider-centric or health organization-centric health record of a person.” (www.infoway-inforoute.ca)
There is also PHR, H/HIS, aEMR, and more. Click here for more details.
Main Functions of EMR
- Health and medical records (consultations, assessments, lab results, etc.)
- Booking system and administrative support
- Task management, team collaboration and communication
- Prescription management
- Decision support and automation
- Research, statistics, data, information
EMR in Vancouver Coastal Health :
Clinical Systems for Allied Health Students
- In progress : CST CERNER
- Patient Care Information System (PCIS)
- Primary Access Regional Information System (PARIS)
- EMRs (Profile EMR, PLEXIA, Input Health, etc.)
EMR in ambulatory clinics Canada
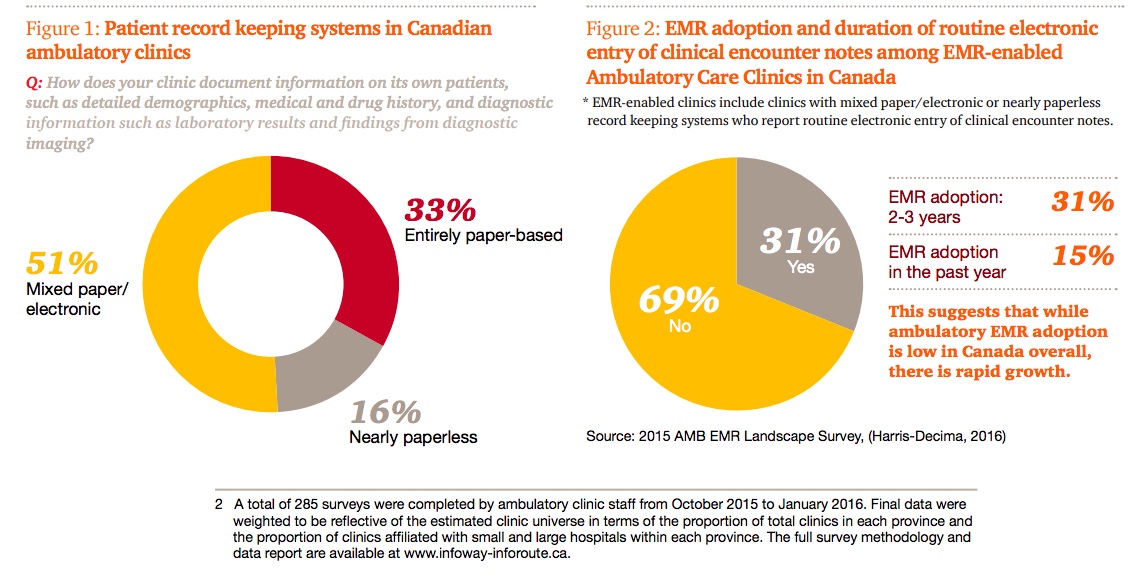
The Emerging Benefits of EMR Use in Ambulatory Care in Canada (2016)
- “Reduced adverse drug event-related emergency department visits leading to hospitalizations;
- Benefits realized by patients when availability of required health information avoids unnecessary delays in care;
- Additional patient visits/clinic volumes as a result of enhanced clinic efficiency through EMR use;
- Reduced staff and clinician time spent on chart management processes, including transcription costs;
- Reduced duplicate laboratory and diagnostic imaging (DI) tests“.
The Case of PARIS and Challenges Around the Privacy of Patient Information
Introduced in 2001, PARIS is an Electronic Medical\Health Record used by Community Health Providers and at Vancouver Coastal Health. It is accessed by staff and contractors involved in the delivery of a wide range of services outside hospitals (community physicians and nurses, SW, Case Managers, OT, PT, and more). The personal information contained within can include notes from all these health care professionals. In 2007-2008 the Office of the Information and Privacy Commissioner identified areas of concern around privacy and decided to conduct a more in-depth investigation. This resulted in the publication of two reports:
Office of the Information and Privacy Commissioner (2010) reviewed PARIS and found: “As a result of our review of the compliance of the system with the standards required by the Freedom of Information and Protection of Privacy Act (“FIPPA”), we found that the privacy protection of personal information in PARIS is inadequate. Major deficiencies in implementation of the PARIS software from a privacy perspective are the following:
- an access model that is team-based rather than role-based resulting in too many users having access to too much personal information,
- several data flows of personal information outside of the health authority that are not authorized under FIPPA,
- the security protection for the system when we investigated it was not reasonable given the sensitivity of the personal information and did not meet the FIPPA standard,
- and records are stored indefinitely – neither archived nor destroyed when they are no longer needed to provide care.
These deficiencies are serious and are a matter of significant concern.”
Auditor General of BC (2010) found that: “Because PARIS users are not granted access on a “need-to-know” basis, sensitive and confidential health care records were accessible to thousands of users who have neither the need nor the right to see the information. Security controls throughout the network and over the database were so inadequate that there was a high risk of external and internal attackers being able to access or extract information, without VCHA even being aware of it. Fundamental controls to prevent or detect unauthorized access to the system were lacking, and monitoring to determine what data exchanges occurred was also insufficient.”
Before EMR – A small team would have access to my personal file

After EMR – A small town has access to my personal file

This raises the question: What about patient privacy and these new technologies?
Let’s look at VCH and privacy
FREEDOM OF INFORMATION AND PROTECTION OF PRIVACY ACT (FIPPA)
BC’s Information and Privacy Commissioner: “I know that frontline decisions have to be made quickly and sometimes the facts may not be as clear as you’d like. But there’s no doubt that privacy laws support disclosures to protect health and safety… if someone uses common sense and in good faith discloses information, my office is not going to come down on them. Privacy is important, but preserving life is more important.” (Source: Privacy at VCH, what you need to know, handout given at staff orientation by VCH Privacy Advisor, 2017).
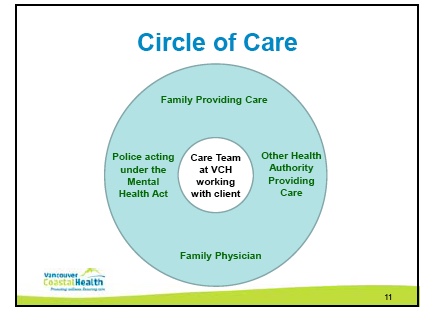
“Staff may disclose Personal Information on a “need-to-know” basis to other health care providers or members of the care team, both within and outside VCH, including to family members who are providing care (i.e., within the “circle of care” or for “continuity of care”). Disclosures within the circle of care do not require consent, although Staff may wish to discuss such disclosures with the Client.” (Source: Information and Confidentiality Policy)
VCH’s Notice to Patients:
“Your information may be entered into our electronic health information systems to assist authorized persons in quickly accessing pertinent information wherever you may be receiving care or services.
“Your health information will be provided to your referring physician, other authorized health care professionals and their support staff, or health care agencies and facilities involved in your care to support continuous and consistent care and service. In some cases, these health professionals may look up your health information in our electronic health information systems in order to provide you with direct or supporting services.”
“If you are a patient in the hospital or residential care, we will provide your family or close friends who phone and ask about you with information confirming your admission and location.“
(Source: Caring for Your Information Notice to our Patients, Clients and Residents, VCH, 2012)
For more information about VCH and privacy: Information Privacy Office
A Look at the College of Social Workers’ Code of Ethics Regarding Consent and Privacy
BC College of Social Workers Code of Ethics
“A social worker shall protect the confidentiality of all professionally acquired information by disclosing such information only when required or allowed by law to do so or when clients have consented to disclosure.”
“Social workers comply with any applicable privacy and other legislation. Social workers obtain consent to the collection, use or disclosure of client information including personal information, unless otherwise permitted or required by law.”
“A social worker shall promote service, program, and/or agency practices and policies that are consistent with this Code of Ethics and the Standards of Practice of the British Columbia College of Social Workers.”
“Social workers keep systematic, dated, and legible records for each client or client system served.”
“Social workers keep systematic, dated, legible records for each client. Social work records include any or all of the following: narrative reports (handwritten, typed or electronic), progress notes, checklists, correspondence, minutes, process logs, journals or appointment records, films and audio or video tapes.”
“Document the client’s situation/problem exactly and contain only information that is appropriate and useful to the understanding of the situation and the management of the case.”
“Report impartially and objectively the factors relevant to the client’s situation. The record clearly distinguishes the social worker’s observations and opinions from the information reported by the client.”
EXTRA: The Social Work Podcast – Episode 113 – On privacy and consent: 2018 NASW Code of Ethics part 1
