By Maura MacPhee
What: Teaching Scholarship/Flexible Learning Workshop
When: February 11, 2015 (1:00-4:00 PM)
Where: Rm T182, UBC School of Nursing
 Guests: Dan Pratt, Jeff Miller, Namsook Jahng, Lucas Wright
Guests: Dan Pratt, Jeff Miller, Namsook Jahng, Lucas Wright
Participants included: Academic/Clinical faculty and teaching assistants from SoN; practice partners from Fraser Health Authority and Providence Health Care.
In a nutshell: We worked in small groups throughout the afternoon—interspersed with large group discussions. We began with a simple exercise to share people’s perspectives of flexible learning: “Create a title/description of flexible learning in 6 words.” The consensus was that flexible learning provides opportunities for teachers to better meet the needs of adult learners with diverse backgrounds at different stages of learning. By the end of the day, participants discovered that flexible learning strategies provide pedagogical and logistical flexibility.
Several nursing faculty contributed examples of how they are using flexible learning in their courses: Joanne Ricci and Ranjit Dhari from community/public health (N336); Farah Jetha and Cathy Ebbehoj from maternal care (N333); Lynne Esson from adult medical/surgical care (N337); Maura MacPhee (myself) from leadership, ethics and policy (N306); and Suzanne Burns from the undergraduate capstone project (N344)—Suzanne is an affiliate faculty with the School of Nursing.
The faculty agreed that flexible learning can be very useful when content is complex and difficult to deliver through lecture; when subject matter experts are difficult to schedule into the students’ tight class schedules; or when specialty courses, such as community health, repeatedly offer the same content in 6 week blocks (e.g., dental health). In these instances, it’s been helpful to use online videos of lecturers or course content that students can watch as many times as needed to familiarize themselves with the content. To assist student learning, these online content/lecture modules need to be accompanied by “guiding questions.” As a follow-up, class time should be used for student and faculty engagement– for deeper discussion, for clarification of any misconceptions.
Dan Pratt stated that this approach allows faculty to use class time for “teaching students about real-world applications” through shared problem-solving (e.g., cases to work through individually/in small groups). Class time should not be wasted through delivery of passive content.
Faculty examples also demonstrated how traditional testing or evaluation is transformed through flexible learning approaches. According to Dan, “testing is re-positioned for learning.” By embedding quizzes and questions in online content or by doing quizzes in class for participation grades, students have an opportunity to gauge their own learning. Formative feedback to students gives them more responsibility for their own learning. Dan referred to this as “self-regulation.” Lynne Esson pointed out how we can use our NCLEX preparatory materials and practice quizzes (e.g., the ATI), to enhance students’ independent learning.
Ranjit shared that when community health lectures were converted to online modules with guided questions and practice quizzes, class time was also freed up for office hours. Since then, more students have come to her with specific learning needs that they have identified on their own.
Dan described how flexible learning approaches complement the theory of “zone of proximal development” (ZPD). The ZPD is a zone where learners grow and develop. This is the zone between what students can do on their own and what they can’t do. In the ZPD, teachers can employ flexible learning strategies (in class, outside of class) that close the gap between do/can’t do. Note: The concept of ZPD is credited to a Russian psychology, Lev Vygotsky.
Lucas Wright and Namsook Jahng from the Centre for Teaching and Learning Technology (CTLT) showed how they have assisted faculty with the redesign of their course websites—to improve navigation and usability of content on these sites. They also provided examples of traditional lecture content that they helped convert into online modules for students to view and re-view outside of class.
Groups shared ideas for incorporating flexible learning into their course work. One issue for further discussion: How can we use flexible learning to enhance teaching in clinical contexts? For students, new grads, continuing education? There was consensus from the group that we need to work collaboratively (clinical and academic faculty, practice partners) for better educational outcomes. Too often-we separate theory from practice. One promising area for collaborative work: deciding on “threshold concepts” for new learners in nursing.
As described by Dan, threshold concepts are absolute or core concepts that transform how people think about a given topic or area of knowledge. What are those threshold concepts that transform students’ perception of nursing? Dan also referred to these concepts as “troublesome knowledge” that students must work through (to become nurses). Dan tasked the group with identifying 2-3 threshold concepts of significance to nursing. In addition, he emphasized that we have a choice: rather than transferring passive knowledge, flexible learning approaches may enable us, as educators, to assist students with knowledge transformation around a few threshold concepts: student transformation to nurses. Note: For more on threshold concepts, see the work of Jan Meyer and Ray Land.
Dan is well known for his work with the Teaching Perspectives Inventory (TPI). http://www.teachingperspectives.com/tpi/. Participants were asked to complete their TPIs to share with Dan during the workshop. Dan provided us with a snapshot of our teaching perspectives profiles-there were two predominant camps: a) nurturing (caring, encouraging, supporting students); and b) apprenticeship (skill practitioners who role model for new learners). Dan challenged us to examine our TPI scores: “Are there incongruities between your beliefs about teaching and flexible learning? “ It’s important to be aware of our own biases and potential resistance to new teaching approaches.
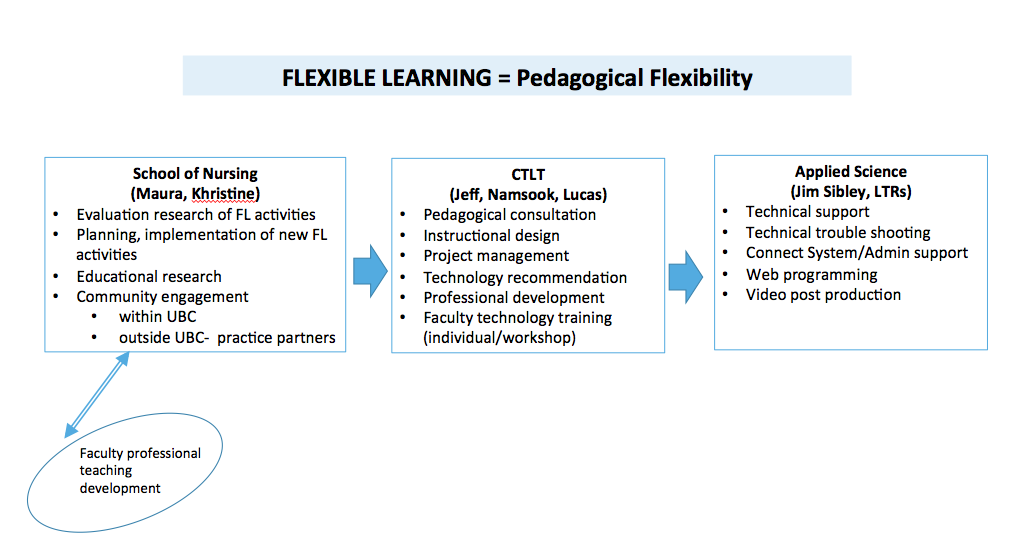
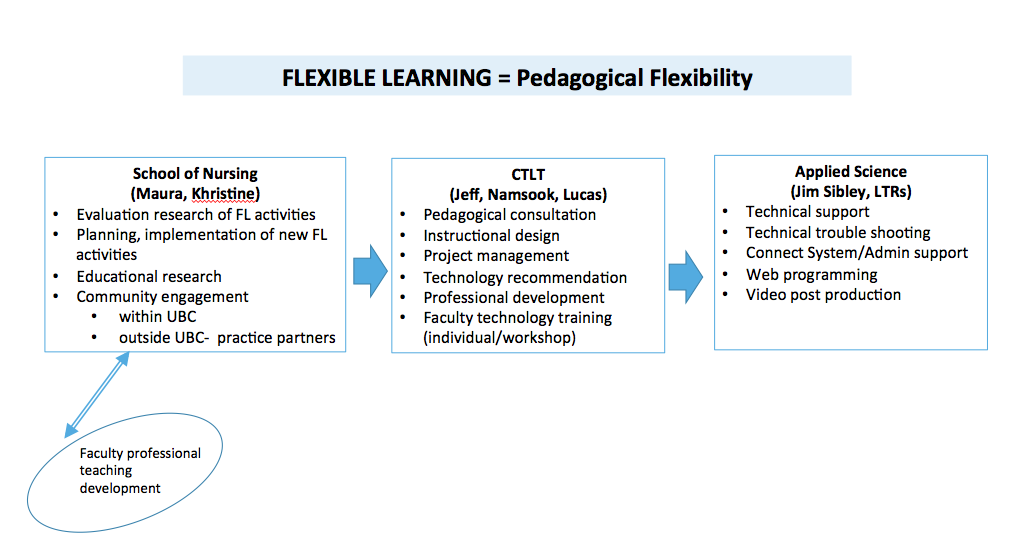
Jeff Miller helped to facilitate discussion about use of flexible learning resources at UBC and we closed with an overview (a flow chart) of supports/resources available in the School of Nursing, the Center for Teaching and Learning Technology, and Applied Sciences (e.g., Learning Tech Rovers). A good place to begin your potential course conversion: contact Dr. Khristine Carinothe, SoN Flexible Learning Coordinator at khristine.carino(@)ubc.ca
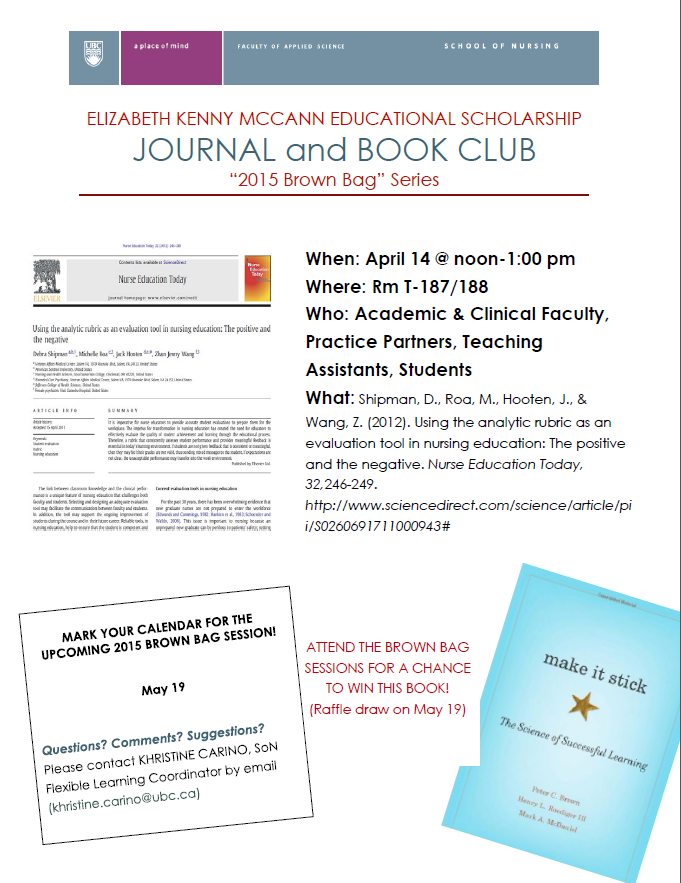
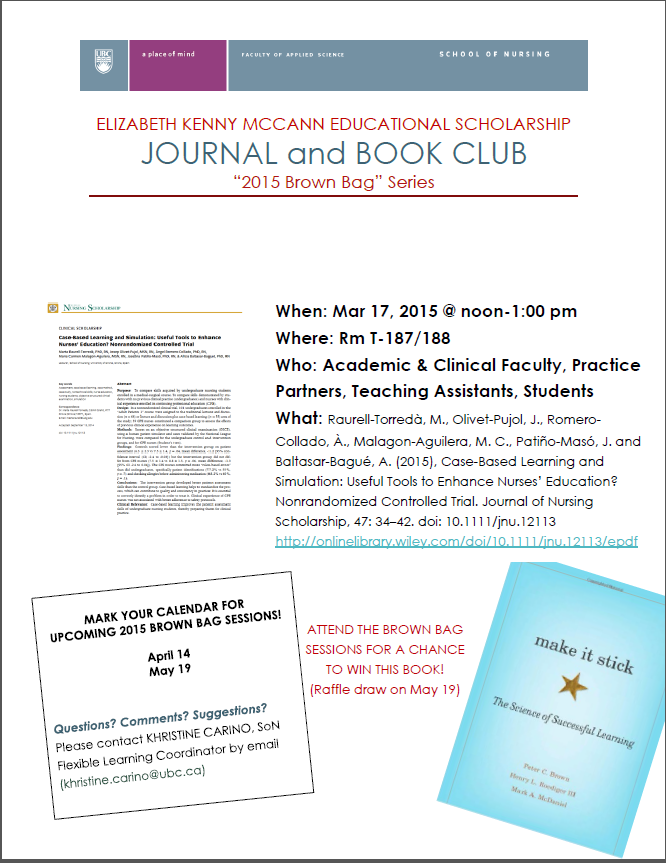
Dan had one final comment—he urged us to check out a book called, Make it Stick: The Science of Successful Learning by Brown, Roediger & McDaniel. Khristine is ordering a few copies of the book to be available to faculty as an EKM resource. Note: Khristine will be setting up a small library of hard copies of articles, books, etc., that she will be housing in T280. We’ll post available resources on the Teaching Matters Blog.
Many thanks to the workshop participants-everyone was engaged and enthusiastic. A great place to begin…