If you’ve ever had some sort of eye surgery, you might have been prescribed an assortment of eyedrops with their own frequent dosing schedules. The reason for the frequent dosing is that topical drug delivery to the eye is quite difficult, and upon further evaluation this should make sense! The eye is a delicate structure that has many barriers to prevent the entry of foreign particles. Hydrogel technology has been heavily investigated as a sustained drug release vehicle, obviating the need for such frequent dosing.
barriers of the eye
Drug residence time delivered via eye drops can be cut short due to pre-corneal factors: tears, blinking, and drainage through the nasolacrimal duct. Some of you might have been told to pinch the bridge of your nose after administering eye drops, this is to block off the drug from draining through this duct into the nose. In addition, drug that does remain on the eye must penetrate through the thick multi-layered cornea to get to the deeper tissues of the eye. The conjunctiva at the surface of the eye is also highly vascularized, meaning the drug will also be absorbed into the bloodstream before penetrating through the eye.
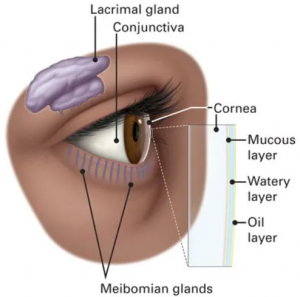
Anatomy of the eye. Credits: American Academy of Ophthalmology
Drainage through the nasolacrimal duct and absorption through the highly vascularized conjunctiva may cause unwanted side effects, as the drug is being distributed to off-target tissues through the circulatory system. Ironically, drugs cannot be delivered via consumption or systemic injection as there are blood-ocular barriers (analogous to the blood-brain barrier) that prevent systemic distribution of drugs to ocular tissue.
hydrogels to the rescue!
Hydrogels are basically polymers (long chemical chains) composed 95% of water. The advantage of hydrogels is that they are viscous, meaning that they can stick onto the eye longer before being removed. They can also encapsulate drug molecules, and can release the desired drug at a certain rate, based on their initial preparation conditions. Currently, there are many types of hydrogels being investigated for there use in drug delivery. These can be broken down into synthetic polymers, which have the advantage of being easily tunable in mechanical properties and natural polymers, which have the advantage of being biocompatible to the eye. In-situ forming hydrogels have been an area of focus, as they can be administered as a liquid, but gels in response to a stimulus. For example a gel could be liquid at room temperature but turn into a gel at body temperature.
Despite being a potential solve to a long-standing problem, there is currently no FDA-approved hydrogel used in drug delivery. A lot more research in terms of in vitro, in vivo, and clinical studies are needed to evaluate the long-term efficacy and biocompatibility of these options. However, hydrogels have made their way into clinical use in other ophthalmic departments! An immediate one that comes to mind is the use of contact lenses which are practically just hydrogels. A lesser known use is in cataract surgery, where hydrogels have been used as ocular adhesives to seal any surgery-induced wounds.
References
Lynch, C.R.; Kondiah, P.P.D.; Choonara, Y.E.; du Toit, L.C.; Ally, N.; Pillay, V. Hydrogel Biomaterials for Application in Ocular Drug Delivery. Front. Bioeng. Biotechnol. 2020, 8, 228, doi:10.3389/fbioe.2020.00228.
