China has Zero Tolerance for Listeria monocytogenes
Did you know that China has a zero pathogen standard that needs to be met for meat imports? Whether raw or cooked, meat and poultry from Canada shipped to China must contain no amounts of Listeria monocytogenes. How would this affect China’s food market and food availability?
Listeria monocytogenes is a facultative anaerobe, meaning that this bacterium is able to survive in environments absent of oxygen. It also has the capability of growing in temperatures ranging from 0 to 40 degrees Celsius. This allows Listeria monocytogenes to grow and to survive on refrigerated and frozen foods respectively. In Canada, presence of the bacteria on food is permitted as long as the detected amount is below 125 CFU/g for category 1 RTE foods and less than 100 CFU/g for categories 2A and 2B. These values were established because foods with less than these detected amounts of L. monocytogenes have low risk of causing illness. In fact, most foods consumed in Canada are usually tainted with L. monocytogenes. According to Health Canada, there is a 0-10% frequency of L. monocytogenes found in RTE foods.
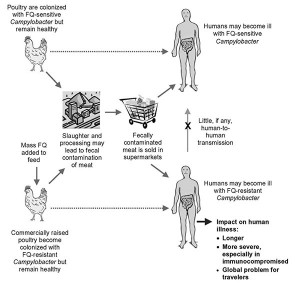
Food from Canada that is exported must comply with the regulations of the country receiving the food, in this case, China. According to the China National Standards (GB 29921-2013), meat products cannot contain any amount of Listeria monocytogenes for every 5 samples tested. If meat and ready-to-eat (RTE) food producers want to export their products to China, they need to apply procedures that would completely eliminate L. monocytogenes from the food. To ensure that cross contamination does not occur, exporters need to follow proper equipment maintenance, sanitation, and handling procedures; however, this may be difficult for Canadian producers to achieve if we export our meat to countries with such requirements because meat can be contaminated through packaging and shipment processes. In addition, there is difficulty in eliminating the bacteria from foods due to the resistant qualities of L. monocytogenes such as sanitizer, acid, and desiccation tolerance, as well as its ability to attach and remain on surfaces.
China’s zero tolerance policy for the presence of L. monocytogenes in meat poses as an issue for other countries wanting to import their meat into China. If China buys meat from Canada and the meat gets tainted during exportation, China destroys the meat. This waste and reduction in food imports is not only harmful to both economies, but also to the food supply in China. Moreover, implementation and regulation of stricter laws is costly.
Compared to previous years, the presence of L. monocytogenes in foods has been increasing. The number of incidences of foodborne infection due to L. monocytogenes reported in China is similar to the numbers from different countries. Since China’s food market is rapidly developing, along with an increase in the population, there is a demand for pre-made, RTE foods. This increased consumption may also mean that there is more risk of infection, but there may also be a lack of supply due to the restrictions on imports. According to the WHO, the likelihood of developing listeriosis depends on multiple factors including how the food is stored, how many times contaminated food is consumed, and the amount of pathogen on the food. Rather than having the zero tolerance policy, perhaps China can consider educating consumers on basic food safety principles.
Considering the risk of infection and the loss of trade, do you think the zero tolerance policy is necessary?
Works Cited
China National Standards (26 Dec 2013). Food Safety National Standard Limit of Pathogens in Food Products. Retrieved from http://cexgan.magrama.es/MODULOS05/Documentos/GB29921-2013-PatogenosEnAlimentos.pdf
Feng, Y., Wu, S., Varma, J. K., Klena, J. D., Angulo, F. J., & Ran, L. (2013). Systematic review of human listeriosis in china, 1964–2010. Tropical Medicine & International Health, 18(10), 1248-1256. doi:10.1111/tmi.12173
Health Canada (1 Apr 2011). Policy on Listeria monocytogenes in Ready-to-Eat Foods. Retrieved from http://www.hc-sc.gc.ca/fn-an/alt_formats/pdf/legislation/pol/policy_listeria_monocytogenes_2011-eng.pdf
Wu, S., Wu, Q., Zhang, J., Chen, M., Yan, Z. A., & Hu, H. (2015). Listeria monocytogenes prevalence and characteristics in retail raw foods in china. PloS One, 10(8), e0136682. doi:10.1371/journal.pone.0136682













 half of the infected people are children younger than 18 years old.
half of the infected people are children younger than 18 years old. 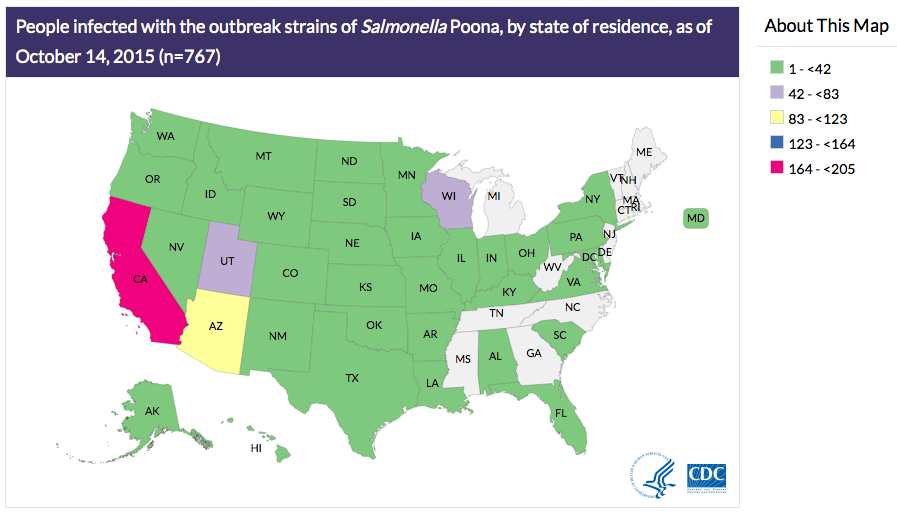
yichen25 10:33 pm on October 31, 2015 Permalink |
I personally think that the zero tolerance policy shouldn’t be enforced in China. There are definitely some pros and cons when it comes to zero tolerance policy of Listeria monocytogenes. The pros being that the meat that arrived in China is much safer for consumption as there are no traces of Listeria monocytogenes, which further decrease the risk of foodborne diseases. However, in this case, the cons outweigh the pros. This is because the implementation of zero tolerance policy will result in less international meat trading between China and other countries and also contributes to more meat wastage as all the imported meats that doesn’t fulfill the requirements will be sent for disposal. China should definitely consider loosening their tolerance policy for Listeria monocytogenes to find a balance that will benefit them the most.
JorgeMadrigalPons 12:56 am on November 2, 2015 Permalink |
I agree with yinchen25. China may be loosing more with this zero tolerance policy. Population in China is really large, thus they must have an efficient food supply system. I think it could be better if the Chinese government focused on informing its citizens about the potencial problems of eating RTE. It is known that Listeria monocytogenes tends to target immuno-compromised individuals, like children, pregnant women, or elderly people, therefore, I think that cutting RTE meats from these individuals diets could prevent potential infections.
angel519 3:50 pm on November 2, 2015 Permalink |
I am surprised to know that China has such a strict policy on import meat produce. I think having a zero tolerance for Listeria monocytogenes is a good approach of preventing foodborne illnesses caused by L.monocytogenes. However, since the number of incidences in China is similar to the numbers from other countries, the governmnet should pay more attention on inspections of post-import activities such as transporting and processing. Even if the imported produce has no L.monocytogenes, inappropriate manufactor practices will introduce the pathogen to the produce. The whole process from import to consumer should be inspected and regulated strictly to be able to achieve zero tolerance and reduce in L.monoctyogenes induced illnesses.
DeniseZhang 9:31 pm on November 2, 2015 Permalink |
I am from China and I did hear a lot of food safety issues in China these years. Maybe it’s due to this “zero tolerance policy”, Listeria is actually not the most reported cause of food-borne illness in the news that I have heard of. I do think a strict regulation is necessary, as there are more and more food safety issues are revealed and reported, food safety becomes a big concern to most of Chinese, as least to those who care about the quality and the safety of the food. After years hearing sever consequences caused by unsafe foods, people were kind of scared and try to seek out foods that come from more reliable source. Therefore I think a strict regulation on Listeria can provide a safety barrier for people in China not just physically but also mentally. Yes, there might be loss in economics, (please don’t judge) but I think food safety is more important for people.
wen liao 4:09 pm on November 3, 2015 Permalink |
It is very interesting that China has such a strict policy on L. monocytogenes while China is one of the countries that has the most food associated outbreaks. However, I do think that it is a good policy especially considering the current status of Chinese food industry. In China, there are many aspects of food production and processing that is not strictly supervised and controlled, which lead to a lot of foodborne outbreaks that should be avoided. For example: the melamine adulteration in infant formula posed a large scandal over Chinese milk industry. Although it is a very strict rule that L. monocytogenes is zero tolerated in China, I have to say that it is better to be safe than sorry.
NorrisHuang 4:17 pm on November 3, 2015 Permalink |
I kind of have mixed feeling about this “zero tolerance policy” because it is being enforced in China and still China has similar number of listerosis cases as the other countries, wouldn’t it be worse if this policy is no longer administered? But I also agree that this policy does affect international trade. Grew up in China, I don’t think much of the food safety cases are related to microorganisms. More of them are related to food adulteration and addition of illegal food additives. And I am also surprised to know that China has such a strict policy on microbial aspect of imported food.
Michelle Ebtia 10:30 pm on November 28, 2015 Permalink |
This is certainly as good as it can get in terms of food safety and risk elimination rather than mitigation. However, as noted by other readers, the costs associated with this policy might outweigh the benefits, e.g. loss of trade. Also, from an international trade perspective, one might wonder if this policy is in place in an attempt to limit the RTE import to china, for example in support of local food production. This assertion might be backed up by a study (Shi et al. 2015) that found 6.87% of RTE food samples in China are contaminated by Listeria anyway!
Work cited:
Shi, W., Qingping, W., Jumei, Z., Moutong, C., & Zéan, Y. (2015). Prevalence, antibiotic resistance and genetic diversity of Listeria monocytogenes isolated from retail ready-to-eat foods in China. Food Control, 47, 340-347.
teewong 11:47 pm on December 14, 2015 Permalink |
I can understand where China is coming from when they imposed the zero pathogen tolerance policy on import foods. RTE foods stand for “ready to eat”, meaning no prior preparations (ex. thermal processing, freezing) are needed prior to consuming, therefore, the chances of getting infected from eating RTE foods are very high! I agree with @emilychow that China should enforce more on educating the public more on food safety preparations, however, in RTE foods, there is really very little we could do to eliminate the pathogen since they are way too tiny to be seen with bare eyes. The most we could do is to throw away the product if it looks spoiled. Listeria monocytogene is also a tricky pathogen since it could grow at refrigerated temperature. I feel it is totally reasonable that they pose a food safety regulation on imported foods.