In July 2014, the parent company of Shanghai’s Husi Foods, OSI Group LLC., recalled all products made by its Shanghai unit as reports arose regarding the quality of their meat and poultry. Investigators suggest that Shanghai Husi Foods, has been selling beef, chicken and pork beyond their expiration date, by repackaging them as freshly packaged products. This isn’t the first time OSI has found themselves in hot water, with similar allegations being brought forward regarding a U.S. based plant by a former employee.
OSI is the major distributor of meats to large international corporations such as McDonalds, YUM! Brands Inc. (KFC/ Pizza Hut), and Starbucks Corporation.
Considering that there are approximately 2000 McDonalds restaurants in China alone, serving thousands daily, the potential impact of this lapse in food safety, could be catastrophic. Michael B. Griffiths, a Shanghai –based qualitative research director at TNS China Co. fears that “this recall may spoil any remaining goodwill consumers have for fast –food restaurants.” According to distributors McDonalds restaurants in Hong Kong and Shanghai are serving a “limited menu” of fish burgers, having pulled Chicken McNuggets, the McSpicy Chicken Filet, and grilled chicken salads off the menu, as these products may contain expired and/ or contaminated meats.
Although no illnesses have been reported, Yum! Brands Inc. will no longer do business with OSI in China, USA and Australia. A McDonalds spokes person also stated that the have stopped sourcing products from Shanghai Husi Foods. The company is in the process of conducting a thorough internal investigation into the possible failures that may have occurred.
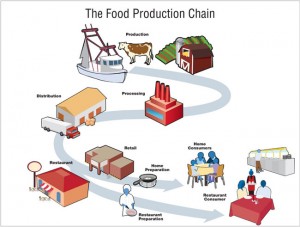
The consequences of meat production failures can be severe and are highly dependent on practices that occur at the processor, distributor, retail, and consumer levels. Failure at any level is unacceptable and can lead to significant economic and health consequences especially in foods with a limited shelf life.
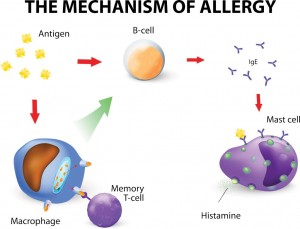
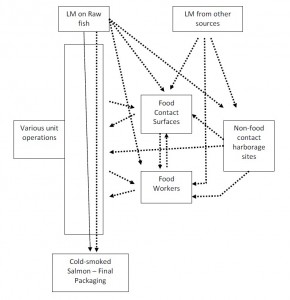
The date marking requirement is put in place and strictly enforced due to the potential of pathogenic organisms to grow at refrigerated temperatures including, Listeria monocytogenes and Yersinia enterocoloctica. Other microbiological contaminates include: Campylobacter spp., E.coli O157, VTEC, Salmonella , and BSE. These pathogenic bacteria can cause illness with symptoms including but not limited to: diarrhea, vomiting, and nausea, highlighting the importance that the date of expiration be accurate.
According to the CDC, businesses should check for the following when receiving fresh meats:
1. Check that the vehicle is clean and temperature controlled
2. Check that the meat products are held at the appropriate temperature (41 degrees Fahrenheit)
3. Reject deliveries if: there is evidence of temperature abuse, off odour or colour, or if meats have a slimy/ sticky texture
OSI Group LLC, is a United States based company with 55 manufacturing plants in over 16 different countries. With the globalization of the food supply market, it is becoming increasingly prevalent for major corporations to obtain their products from outsourced processors and distributors. With this in mind, consumers and retailers must be cautious when purchasing meats and should only do so from trusted distributors. Furthermore, it is important to know WHERE in fact these products are coming from such that in case of an outbreak, measures are in place that, allow retailers to retrace their steps.
The bottom line…
Regardless of the date of expiration on these products, consumers (including those that are commercial) should ALWAYS check for signs of spoilage and take the appropriate measures to ensure that these products are discarded.
For more information regarding Food Safety, feel free to check out: http://www.cdc.gov/features/befoodsafe/
Works Cited
Bora, K., International Business Times ( 2014). http://www.ibtimes.com/china-food-scandal-osi-group-recalls-shanghai-husi-made-meat-brings-new-management-team-1640430
Bloomberg News. (2014)http://www.bloomberg.com/news/articles/2014-07-28/mcdonald-s-supplier-recalls-meat-in-expired-food-scandal
Centre for Disease Control. (2015). Food Safety Training. http://www.cdc.gov/nceh/vsp/training/videos/presentations/foodprot.pdf
Center for Disease Control (2015). Fighting Bacteria http://www.fightbac.org/food-poisoning/causes-symptoms/
Kansas State – Meat Safety Video (2015). https://www.youtube.com/watch?v=qced9Du_3gc
Wang, S. (2015). Lecture 14 : Meat Safety. FNH 413 Food Safety