All posts by rachelle fulford
Rough start
Today started out with a 30 minute resuscitation. It’s not my favourite way to start the day, but Lesley and I were working so well together and we had good bilateral air entry right from the start with a steady (if a little high) heart rate throughout.
Thank you thank you to all who donated toward resus equipment! It truly saves lives!
After 30 minutes the baby boy started breathing on his own and the Pediatrician assessed him and gave him a dose of antibiotics. He was stable for the time being, but we are going to check in on him over the next few days.
The rest of the day was filled with more births! (Imagine that!) we had a precipitous multip birth (one push and the baby came right out!), a slooooooowwww primigravida birth, another slllloooooooowwww primigravida birth, a speedy speedy multip birth in the admission room and an unexpected breech in the first stage room (Lesley and Beatrice worked wonders with that birth in not so ideal circumstances.)
I am continuing to learn a tonne, and my gratitude grows everyday to these mothers and to my midwife teachers.
Birth is wild. Women are strong. Babies are resilient.
Cathy’s comment from “In Labour & Delivery” Gallery Post
Cathy – our fabulous instructor – posted a comment to our most recent gallery post. I tend to be a bit ‘wordy’ with my posts, and thought Cathy’s succinct summary of the past weeks was deserving of it’s own post!
—
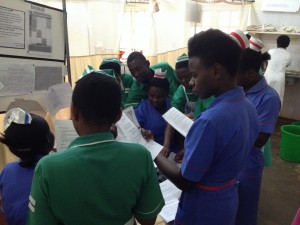
“I have two more clinical days to work with Rachelle and Lesley at Masaka Regional Referral Hospital. We have dealt with every emergency in our Midwives Emergency Skills Course, as well as the “Advances in Labour and Skills Management’ (ALARM) course. This includes breech, twins, excessive bleeding before and after birth, hypertension, pre-eclampsia and premature deliveries. We have also attended older moms, 15 year olds, and worked alongside many Ugandan students who did not have preceptors with them and whose skills were at beginning levels. Shortage of supplies and human resources are the norm and there is always too much work to do. Our students are loving and caring to the mothers and will be strong midwives for women and families in British Columbia.”
Cathy Ellis, RM and UBC instructor
“Whoop – there it is!”
Today was my second day back in the delivery room after twelve days! We spent a weekend in Jinja (where I focused on white water rafting on the Nile!) followed by a week in Kampala (where I focused on antenatal assessments, observing fistula surgeries, and teaching workshops) followed by a weekend at Lake Mburu (where I focused on taking photos of zebras, leopards, and hippos!), followed by a virus that kept me in bed for a day. My first day back (yesterday) was quite interesting – my first ever 5x nuchal cord (cord was wrapped around the baby’s neck five times!) as well as my first experience of cord prolapse (Having to hold the baby’s head up off the cord while we rushed the mother to the OR was crazy hard to do! We had a positive outcome, though, and there was much cheering in the OR!) It’s been great to get back into the swing of birth.
Today:
1st STAGE ROOM BIRTH! The birth in the first stage room was totally unexpected. I went in to do a simple “early assessment” of a 15 year old primigravida (first pregnancy): palpation, fetal heart rate, maternal vitals, contraction pattern, and vaginal exam. After palpating mom’s belly it seemed her bladder needed emptying. She was unable to pee, so before I proceeded with anything else I catheterized her. As I did so I noticed her pushing… and… the baby’s head suddenly appeared!
“Whoop – there it is!” (lol!)
I was totally unprepared for birth, but Lesley was on it! I was already “sterile” from having just catheterized her so Lesley (who had been assessing a woman with severe hypertension also in the first stage room) speedily gathered the supplies we needed for birth: 10 iu oxytocin in a syringe, cord ties & a razor blade, baby blankets. The mom was 15 years old and her body was noticeably smaller than other women I’ve delivered. Her perineum was only about two centimeters long (short!) and I have to admit I was a bit nervous.
The second stage proceeded quite slowly (the stage where a woman is fully dilated and pushes her baby out), but when the baby girl was finally born she came with double nuchal hands – both her hands were in fists around her face! No wonder her head was slow to emerge! She came out pink and crying, and the placenta came (complete) a few minutes later. She did have a small first degree tear to repair, but overall it was a lovely birth!
TWINS! The twins were, as with the first birth of the day, unexpected (to me). I had just finished telling Cathy that I was starting to feel unwell and thought I should probably head home. I had stayed home sick the day before and suddenly felt the sickness returning. Cathy thought that was probably a good idea, but asked that before I left if I would insert an IV on the mom who had just arrived – a G3P2 pregnant with twins. We had just assessed her as 6 cm dilated and we wanted to get the IV in before we left. Women pregnant with twins are at increased risk for PPH (post partum hemorrhage) due to the distension of their uterus from carrying two babies, and being prepared with an IV can facilitate giving medication quickly should bleeding occur postpartum. Cathy asked me to do it because we have a little skills game we like to play called “3 for 3”. I had successfully inserted two IVs that day, and this would be my “3 for 3!”
I happily agreed.
A few minutes later, after having successfully setting up my “3 for 3” IV, the mom looked at me and simply said, “Omwana” (ie. baby). I lifted up the mom’s dress and again…
“Whoop – there it is!”
A baby was coming! She had dilated from 6 to 10 in about 15 minutes! My call for help came out like this: “Baby, coming out, now!”
Thankfully Cathy and Lesley were both free to come to my aid. In less than 10 seconds Cathy brought me sterile gloves to put on top of my nonsteriles and drew up two doses of oxytocin, and Lesley went to track down the woman’s baby blankets. (The hospital here does not supply blankets to receive babies; the women must bring their own. In this case this woman had neglected to bring her supplies with her into the delivery room, and it can take a while to track down her attendants out in the hallways/front lawn to get her supplies!) The baby was born very quickly so I grabbed the mom’s personal shawl to warm and dry the baby. “Twin A” was screaming just as we like, and though Lesley returned without having found the woman’s attendant and supplies she was able to retrieve one of our donor blankets from the storage closet to wrap the baby in, which was awesome. (Thank you donors!!!)
The thing about a woman birthing twins is that Twin A needs to have their cord cut and clamped right away. With single babies we prefer to do delayed cord clamping. This ensures the baby receives maximum blood post birth and reduces rates of anemia at the 6 month mark. With twins, though, you have to be careful. We did not know if the babies shared a placenta and amniotic sac. If they did, something called “twin to twin transfusion” can occur, and if the first twin continues to take in blood from the placenta after it is born there is a possibility that the second twin can lose too much blood. Because we were not prepared for the birth we didn’t have our clamps handy… but… I had clamps in my pocket for just such an emergency! Thankfully! I pinched the cord and Cathy went digging in my pockets and found two clamps. Perfect. We clamped the cord, cut it, and Lesley went off with baby to the warmer while we prepared for Twin B.
The next step with twins is to determine the position of the second twin. We palpated and could tell the baby was in a longitudinal position, which was good. If there’s one thing you don’t want it’s a baby in transverse lie. According to our palpation the baby was breech, and as I did a vaginal exam to confirm our suspicion I felt a foot. Alarmed I looked to Cathy and said, “It’s a foot! What are we going to do?” (I have it lodged in my mind that a baby in frank or complete breech are fine for vaginal delivery, but footling can be a problem.)
Cathy, in her calm and witty way, looked at me, smiled, and simply said, “It’ll come out!”
Sure enough not 5 minutes later Twin B’s two feet slid out of mom’s vagina – IN THE CAUL! I have never seen that! Breech-in-the-caul! Amazing.
We opened up the sac and proceeded to have a vaginal breech delivery. I remained hands off until I could see the scapula. Then I reached in and scooped out the anterior arm, rotated the baby slightly in the opposite direction by placing my fingers on the iliac crest and my thumbs on the sacral bone and rotating, and then scooped out the other arm in the same way. Then I got into the mariceau-smellie-veit-position with the baby resting on my left forearm with my two fingers on the baby’s mallor bones just inside the introitus and my right hand provided flexion on the occiput. This was only my second breech delivery, and I found this move much harder this time around! We had to ease the baby’s head out by rocking it quite a few times – something I don’t remember being taught in our training and I was so glad to have Cathy’s extensive experience at my side. Baby was born, and though a little slow to breathe at first, he came around within a minute and no resus was necessary.
With the birth of Twin B came a gush of blood and the placenta was right there – there had been a placental abruption! (And boy were we glad we had the IV already inserted!) We gave the mom 10 iu oxytocin IM as well as 10 iu oxytocin IV in 500ml Ringers lactate. We removed the placenta (monochorionic/diamniotic for those of you interested!), rubbed her fundus, removed clots and catheterized her bladder with an in-and-out. The fundus firmed up nicely so we quickly assessed for tears and found a small first degree tear that needed suturing.
All in all, another amazing birth and the mom was delighted with her boys.
During the excitement I had been able to put my feelings of sickness aside… but shortly after the delivery of the placenta and initial postpartum management I started to feel unwell again, so Cathy encouraged me to head out and she would finish up. I was grateful to be part of such a supportive team!
When Cathy and Lesley returned to our accommodations a few hours later they told me that the mom had started to bleed again after I left. They expelled numerous more clots and had to give another 10 iu oxy IV as well as 600 mcg misoprostil. Although we had used an in-and-out catheter, it wasn’t until they actually inserted a Foley (a catheter that remains inserted to continually drain the bladder) that the uterus fully firmed up and the bleeding stopped. Foley’s are in limited supply here in Masaka so we had been hesitant to use one at first… but lesson learned. In the face of bleeding when risk factors are present, get the Foley in if you have it…
What a day!
Cathy’s Survival Tips
because you never know when you’ll need them…
- When you encounter a lightening storm, throw your pack on the ground and sit on it.
- When you are confronted by a boa constrictor (or other large snake), stand with legs wide apart so it can not wrap around both legs and knock you over. When it wraps itself around your one leg (because it will), stab it with something sharp. Snakes fear pain.
- When you are chased by a hippopotamus, run in a zig-zagged fashion. Hippos run in straight lines and you will outsmart it.
- In the event of an earthquake, duck and cover. Or, if you are in an unstable building, move quickly to an open area. Do not stop to grab computers.
- In the aftermath of an earthquake, be prepared! Have your bag packed with important supplies (eg. shoes, food, phone) and be ready to leave the building in under 30s.
- The most important survival equipment is… water drops. Never, ever forget to bring your water drops.
(And the second most important item? – A fully charged phone!)
In labour & delivery
Reflections at the 2-week mark (is that really all it’s been?!)
We have now spent two weeks in Masaka Regional Referral Hospital. Some shifts have been light, but many have been tough – for a myriad of reasons.
- The air in the delivery room is hot, and made hotter by the heavy plastic full-body aprons we wear to conduct births. My hands are constantly wet from sweat from the double gloves I have to wear to keep protected due to high rates of HIV. My “birth goggles” are constantly fogged up and I can’t even count how many times *a minute* I wipe the sweat off my face on the sleeve of my shoulder.
- The smells are strong: body odour is thick, birth smells are amplified in the heat, and somehow the placenta container lost its lid this week! One woman yesterday had chorioamnionitis and I have never, ever smelled anything so foul. The room smelled for the rest of the day and we all felt like we could taste it. Ugh.
- The floor is… not clean. Squeegeeing all the fluids across the cement delivery room multiple times each day is the least fun part of… everything. [Lesley disagrees – she thinks the spraying fluids is worse! She’s had multiple pphs or bursts of amniotic fluid *across the room* most days!!!]
- I am constantly, constantly learning. Every moment on the ward is a moment to take something in and when we return home each night I am wiped out.
- The systems in the hospital can be frustrating. I won’t go into the specifics of these, but everyday I’m baffled by some aspect of organization. But…. I am in a different culture, and each and everyday I have to remember that.
- I am in a different culture, and the rules are different here.
In the midst of the challenge there are spurts of joy.
- Cathy is hilarious, and always up for fun. After our first day in the hospital I asked if we could buy hand towels so we could dry our hands after washing them (rather than wiping them on our filthy scrubs). Cathy bought brightly coloured towels and promptly named them our “victory towels”, which we wave when good things happen on the ward!
- Bababz the cleaner shoulder-checks me in the mornings to greet me, and gives me the fist-to-fist greeting throughout the day. Hilarious.
- Alice the midwife makes me smile the moment she walks into a room. She is always ready for cheer and is so, so helpful.
- The colours of the birds are incredible – yellow, purple, blue, red. We walk ~15 minutes to hospital everyday and it’s delightful to see incredible flora and fauna all about – especially the ugly storks outside the maternity ward.
- Neonatal resuscitation works!
- The people LOVE it when I use my Lugandan phrases. “Wasuzoteea!” “Kah-ley!” “O-lee-o-tee-ah!” “Whey-bah-ley!” I *love* their smiley reactions!!
- The women amaze me each and every day. What they face in daily life – and in birthing their babies – requires resilience, courage, and strength. They teach me what is possible, even though I don’t think they should have to face what they face.
Tonight I am tired, and to be honest, I don’t feel like going in to the hospital tomorrow. Witnessing first hand maternal-infant health in Uganda has been eye-opening, challenging, and an incredible opportunity to solidify my knowledge and skill. But it’s hard work. Standing on the threshold of the delivery room you just don’t know what awaits you inside.
- Will you be confronted with a woman who received bad care at one of the local private clinics? Or a woman who took “the native” – local plants to speed up labour, unknowingly at her baby’s expense? Or will she have paid someone to give her a shot of oxytocin or a few pills of misoprostol to do the same?
- Will you find a woman who has been laboring for days, but because her lack of nutrition as a child her pelvis did not grow wide enough to allow passage of a baby?
- Will there be a woman whose water broke 4 days earlier and she is now overcome with infection?
- Will a baby die today? Will a mother?
I have learned to look closely at the codes for my clients to know if they are HIV+ or not; many are positive. Today a 17 year old HIV+ mom gently asked us to make sure her baby would get treatment, and another 20 year old asked us not to let her attendant know her positive status.
When you are not used to them, these realities take a toll. I have only been here for two weeks. Two weeks. The midwives here face these stories – these women – day after day after day. And they are tired too. They are paid for 8 hour shifts, but are required to stay for 12 hours.
This weekend is our retreat weekend with the Mbale team. We’ll meet up in Jinja and have some fun together – and I am ready for a break! We will also have a clinical “case study” academic exercise and go through our midterm evaluations. Next week we’ll be in Kampala at Mulago National Referral Hospital facilitating teaching workshops and participating on various antenatal and delivery wards. I look forward to a change of pace. After that we’re back to our respective sites in Masaka and Mbale for until we head home early July.
Time is passing so quickly and so slowly at the same time. It’s sometimes overwhelming and sometimes super gratifying. But for right now, I’m so happy to be going to bed.
Conversations
With the head midwife
Head midwife pops in to see how things are going in the labour & delivery ward. Cathy and Rachelle are attending a woman in 2nd stage to deliver her baby. No other midwives are present in the ward.
Cathy: “We should let you know that we will be leaving after this birth, but the two women in Beds 2 & 3 are about to have their babies.”
Head midwife [as she walks out of labour & delivery]: “We shall pray for them.”
Between head-midwife and student midwife
Student midwife: “There is no stretcher to take this woman to theatre.”
Senior midwife: “Midwife – walk your woman.”
With a labouring woman
Winnie: “Sista – help me!”
Rachelle: “I’m here.”
W: “Help me.”
R: [puts counter pressure on laboring woman’s back.] “I am here. You are doing great.”
W: “I’m dying!”
R: “You’re not dying. You are having a baby!”
W: “When?”
R: “Today! You will have your baby today.”
W: “What time?”
R: “I don’t know what time!”
W: “Tell me when my baby will come!”
R: “I don’t know what time, but it will be today.”
W: “I’m dying!”
R: “No, you are not dying. Here is some sugar-tea. Do you think you can lie on your side?…”
W: “Don’t leave me!”
R: “I won’t leave you.”
[Baby is born about 45 minutes later.]
W: “I am so happy. Thank you. I am so happy.” [Big smiles.]
R: “I am so happy too!
With a stranger at the bank
After a friendly exchange with a Ugandan woman at the bank…
Friendly stranger: A man once said to me, “You are strong like a man.” But I said, “You are mistaken. I am woman.”
The Folic Acid Emergency!!!
We had such a funny moment yesterday.
One of the student midwives here – Samuel – has been a great help and keen learner. At the end of the day he came running into the delivery room where Mickey and I were wrapping up with a delivery desperately calling out, “We need folic acid!”
I came out from the behind the curtain looking at him with a confused look on my face. I totally didn’t understand why he was so desperate, and he said it again, “Rachelle, we need folic acid. You must get it.”
I had the key to the cupboard where all the supplies are locked up. So I asked him, “Who needs folic acid?”
S: “Your colleagues are asking for it! They need it quick!”
R: “Where do I get the folic acid?… and wait… this is strange, why are they so needy for folic acid?! lol!”
Not wanting to leave anyone waiting for their emergency folic acid I rushed across the hall to find out what was going on and Cathy yells to me –
C: “We need a Foley catheter!”
I had to laugh (even though their need for the Foley was no laughing matter. They were in the midst of a cord prolapse for transerse lie with arm presentation and needed the Foley to retrofill the woman’s bladder to help keep the baby from descending any further.)
I rushed back to the delivery room, unlocked the cupboard, and grabbed a Foley – but before I rushed it back to where Cathy was I showed Samuel the package where it was clearly labeled “Foley Catheter”… and he burst out laughing.
Gotta love 2nd language mishaps.
#1 Days 1 & 2 at Masaka Regional Referral Hospital – Overwhelming!
We’ve had two days of work at the Masaka Hospital. Cathy told us she would ease us in with a couple of “easy days” before we start working normal shifts… but she lied to us! They were full, full days – the second we even categorized as “a very hard day.” So far I have had 5 births as the primary attendant including: twins, breech, two pph’s (post partum hemorrhages), a retained placenta, a shoulder dystocia, and sadly a neonatal death. I’ve also assisted with some of the births that Lesley attended (which I’m sure she will write about at some point too!!), and heard a few happening behind the curtains separating beds – I think two births happened on either side of me as I was attending the twins!
The neonatal death was hard. The baby died about 20 minutes after she was born. When the mother’s water had broken there had been meconium present, but she did not come to hospital until 4 days later when she was in 2nd stage (the pushing phase). We rushed her into the delivery room. The head birthed very slowly and I recognized “the turtle sign” right away – the baby’s head shrunk back in turning purple as it did so. The baby had a double nuchal cord around her neck as well as a shoulder dystocia. The lead nurse Prossy helped me deliver her (after I did McRoberts and Woodscrew she stepped in and I’m not quite sure what she did but the baby came!) The baby was born limp and did not respond to positive pressure ventilation (resuscitation), which we performed for ~20 minutes. Additionally, the suction equipment here is broken, and they actually do not have the capacity to intubate for deep suctioning in the delivery room. We suspect the baby succumbed to meconium aspiration deep in her lungs. Meanwhile the mom started to hemorrhage and had a partially retained placenta. We administered 10 IU oxytocin IM as part of active management of the third stage, and another 10 IU oxytocin IV in 500 mls of normal saline to help the uterus contract and stop the bleeding. We also catheterized and emptied her bladder and then Cathy took over and manually removed the placenta, which is a painful procedure (and the situation here is such that there is no option for pain medication.) This whole birth was difficult for me, and I had to take a few moments in the corner to shed a few tears. But then I had to buck up and carry on because there wasn’t a single moment between our 10am to 6pm shift when there wasn’t a woman about to birth and several more in the hallway. In fact, Lesley caught a baby in the assessment room, and a few of the other Ugandan student nurse-midwives were catching other babies in the assessment room as well because the delivery room and it’s three beds were constantly full! (((But with so many students & midwives helping women in the assessment room there were several times the delivery room lacked any staff at all, leaving women unattended during the very time when they needed attention most.)))
One of the biggest questions I have come to Uganda with is the question of ethics: is it ethical for me to be here? This question is important as I make decisions about future goals, and I didn’t feel like I could answer it without coming and seeing first hand. Tonight as I consider what I have seen so far, this is where I’m at: One of the ethical concerns I think about is whether a woman actually has a choice in whether to have me, a foreigner, as part of her labour or not. For some my white skin represents a colonial past they want to forget. For others my lack of the local dialect inhibits the full scope of care I can offer. And for others, the fact that I am a student in need of a preceptor to check everything I do may involve more meddling than they want. But. From what I’ve seen so far (and yes, it has only been two days…) – this is the wrong question. Choice is important, but maternity care in Uganda is *so far behind* what we have in Canada and birth is literally a life and death situation for many of the women who come to the hospital. And, the resources here (including staffing, equipment, and medication) are in such short supply that if we (Canadian midwives and students) weren’t here several of the women we attended these past few days would not have been attended at all.
The non-glamourous truth is that women arrive at hospital with a plastic sheet to put on one of the three plastic covered “beds”. By the end of their delivery they are often soaked from their own blood, urine, and amniotic fluid – and there are no cloths to offer them to clean up. We are not able to get them a clean sheet or even a pad to go in underwear if they have underwear. The last woman I attended yesterday had a few cotton balls worth of cotton baton left from her “mother kit” after her birth so I used it to wipe off a small corner of her wet back – but it was a pretty useless move on my part. She had to head over to the open shower in the corner to wash off (and there is often no soap), and while she was away we poured bleach on the cement floor under her bed and squeegeed all the blood to the drain at the side of the room, and wiped down her bed in preparation for the next woman to come in.
Many women come from villages, and they are coming to hospital because they are experiencing problems. As I learned from the video about “Mrs. X” (see here if you are interested) one of the biggest concerns for maternal and neonatal mortality are the “3 Delays” – the delay to recognize a problem in pregnancy/labour, the delay to get to a hospital, and the delay for the hospital to act (usually due to lack of staffing/supplies). In fact yesterday morning a woman died in the labour ward having suffered from an antenatal bleed that started at home 4 days earlier. She was a Gravida 12 (had been pregnant 12 times prior) but by the time she got to the hospital there was nothing that could be done for her. She was somewhere between 26-32weeks, and her baby was stillborn. Prior to her death I attempted to get her blood pressure, but I was unsuccessful because it was so low. She was given a unit of blood but it was too late.
Today I don’t think it’s unethical that I’m here. I’m a student, but I have come with Canadian preceptors who hold me to Canadian standards. The women don’t get to choose me, but together we bring skill and care that many women would not receive were we not here. Every birth I have been a part of so far has ended with the mother thanking me for helping her. I don’t know. I might not be seeing all the issues yet. But I do know that when we left tonight the head midwife said to Cathy, “You saved that woman tonight” (referring to a case I wasn’t a part of, where a woman had a severe pph and retained placenta but Cathy got it out during the long wait for the OR.) Many of the women coming to hospital are coming because there are problems, and skilled help makes a world of difference for them and their families.
I’m going to need more time to flesh all this out, and to form solid opinions, so bear with me in the posts to come! There is going to be a lot to process as the weeks move on. We’ll do our best to keep you updated, but the days are long, our internet is sporadic, and we are already tired! But the pineapples and avocados are still amazing, and they are going to help me process everything too 😉
***I’m posting this now after our third day at hospital. I had another baby born who wasn’t breathing at birth, but today our resuscitation efforts were rewarded with a baby who came to, is breathing, and we have every reason to believe is going to be a-ok. That feels good.