Ah the clinical stuff has begun! My favorite to learn, even though most of these things – not so yummy to learn about and see though
Let us start with… Leprosy!
What do you think about when you hear Leprosy? I always think about the colonies where it is severe and the people have no fingers and toes, or noses or have holes in them because of the scary movies you see when you are little and they have the leper colonies of evil, scary people limping around. – I have no idea what movie my parents let me watch when I was little that scarred me for the rest of my life like that but that’s what I always think when I hear leprosy..
There is a variety of symptoms associated with leprosy, a few include numbness of the skin, Erythema Nodosum symptoms = painless rash developed over the last couple months without itching, sarcoid on the skin (discolouration), and many more that will be brought up throughout. But what is Leprosy? Is it a skin disease, an infectious disease, a neurological disease? What is the etiology? Well.. really it is all of the above. It is an infectious disease that can cause severe, even disfiguring skin sores and nerve damage to the arms and legs. It however is not THAT contagious as we originally thought, you need to come into very close, repetitive contact with the bodily fluids (usually from the nose or mouth) of someone with UNTREATED leprosy.
Leprosy comes from a bacteria called Mycobacterium Leprae (M. Leprae). Again some symptoms include disfiguring skin sores, lumps or bumps that can last for several weeks or months. Nerve damage, affecting the skin and peripheral nerves. The eyes and inner lining of the nose can also be affected. Loss of feeling in the skin in the arms and legs and muscle weakness associated with the numbness as well.
- 3-5 years is a typical incubation period for symptoms to appear, some don’t even experience or develop symptoms for 20 years – the bacteria is THAT SLOW.
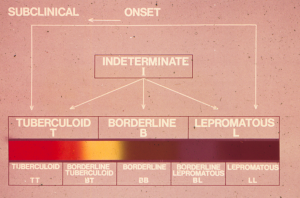
There are actually a few different types of leprosy, dependent on symptoms and each need a specific treatment. The types include:
- Tuberculoid: a mild, less severe form. Usually only showing with one or a few flat, pale-colored skin patches. Numbness of the skin due to nerve damage under the skin may occur as well. This type is also one of the less contagious forms.
- Lepromatous: a more severe form. It has widespread skin bumps and rashes, numbness and muscle weakness. The nose, and kidneys can be affected. This type is more contagious than tuberculoid.
- Borderline: This is really just when you have symptoms of both the above forms.
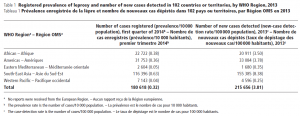
Global Leprosy Trends (all types) Incidence: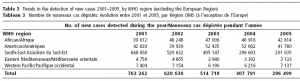
Prevalence 2005 219 826
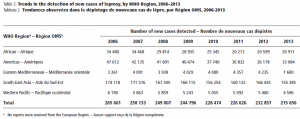
Prevalence = Incidence x duration of disease
Prevalence 2013 180 618
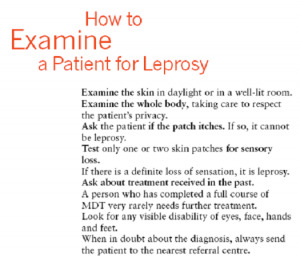
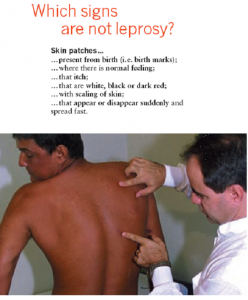
When looking for Leprosy –
Notice the line “Ask the patient if the patch itches. If so, it cannot be leprosy. The patches that appear actually do not itch, they are also painless. This is important! Another thing to point out and highlight is “Look for any visible disability of eyes, face, hands and feet” – this could be very important for catching the bacteria before any severe symptoms occur and loss of limb occurs.
How to classify Leprosy? How to treat?
Leprosy is curable! BUT important to diagnose it early AND to treat complications rapidly to avoid disability
- Classified into Paucibacillary or Multibacillary leprosy dependent on the number of patches the patient has.
- 1-5 patches – Paucibacillary – treat with 6 PB blister packs
- Rifampicin: 600 mg once a month
- Dapsone: 100 mg daily
- Duration: 6 months
- More than 5 patches – Multibacillary – treat with 12 MB packs
- Rifampicin: 600 mg once a month
- Dapsone: 100 mg daily
- Clofazimine: 300 mg once a month and 50 mg daily
- Duration: 12 months
- Single skin lesion Paucibacillary
- Single dose of:
- Rifampicin: 600 mg
- Ofloxacin: 400 mg
- Minocycline: 100 mg
- Single dose of:
- 1-5 patches – Paucibacillary – treat with 6 PB blister packs
Complications: nerve damage! – Very important that you examine the patient and reduce the dose of corticosteroids every two weeks.
- Need urgent action:
- Must be seen by a health worker
- Paracetamol/aspirin for pain
- Steroids
- Maximum dose of Prednisolone is 1 mg per kg of body weight
NEXT
Intestinal Helminths – worms… we learned about worms. (like the microscopy – so many worms, so disgusting and oh so graphic.. there was a warning sign before the lecture slides started saying “Warning – This lecture is likely to contain extremely explicit visual material”)
Epidemiology:
- More than 2 billion people are affected by “soil transmitted helminths” and 300 million have severe morbidity resulting from this. Although most infections are light and asymptomatic, therefore the prevalence of infection is not really a useful parameter of disease.
Significance:
- Negative effects on nutritional status, growth, cognitive processes and school performance
- High prevalence among school children (400 million out of 1200 million infected)
- Treatment can rapidly reverse these negative effects and the treatment is really just a single dosage of cheap drugs! (which is perfect for developing areas that are poor or in poverty)
- Imidazol-drugs:
- Mebendazol – 100 mg tablet for 3 days or 5 all at once (500 mg total)
- Pinworms: 100 mg for 3 months
- Albendazol – 400 mg tablet – one tab
- Ascaris/hookworms – 1 tab for 1-3 days
- Tricuris – 3 days
- Ivermectin – 3 mg tablets for strogyloids sterchoralis
- Normal host: 200 micrograms per kg for one dose
- Immunocompromised: 200 micrograms per kg on days 1, 2, 15 and 16
- Mebendazol – 100 mg tablet for 3 days or 5 all at once (500 mg total)
- Imidazol-drugs:
Common Soil transmitted helminths:
- Trichuris trichiura (whip worm)
- 10-15% of 2-6 year old children have Trichuris with symptoms of colitis and stunting of growth
- With treatment – 85% of the totally parasite population is cleared and 80% of the infections with more than 100 worms per person (ew.. could you imagine being told you have more than 100 worms inside of you.. Ah!)
- Enterobius vermicularis (pin worm)
- Ascaris lumbricoides (giant intestinal roundworm)
- . oh so graphic – I will let you google that one for yourself. But these worms are the size of the worms you find in your garden, now imagine about.. 20-100’s of these coming out of you (out the back door).
- Anchylostoma duodenalis/Necator americanus (hook worm)
- Strongyloides sterchoralis (threadworm)
Worm Biology – useful to know for microscopy and testing
- Pre-patency period: the time necessary for ingested eggs to develop into adult worms capable of producing eggs (ex: Ascaris is approx. 3 months)
- Lofflers syndrome: Migrating, spontaneously resolving lung infiltrates and often eosinophilia and hyper IgE
Diagnosis of intestinal parasites? Well it is hard to really test but you can get a suspicion from a few things such as, eosinophilia ( an increase in the number of eosinophils in the blood – commonly occurring in the presence of parasites), high prevalence area (look where you are, is this common? Did they come from an area of high prevalence, did they drink the local water or eat the local food without knowing where it had been or if it was washed, etc), and look at the symptoms (do they have a belly ache, upset feeling in the intestines and bowel, anemia, suggestive rash).
- Testing: Testing the stool for Ova and Cysts – direct microscopy (we learnt about this in the microscopy lectures and practical session), concentration techniques (ether-formol) and culture tests (only strongyloides – seen just underneath the skin [picture below]). My favourite – scotch tape test. I am 100% serious it is a test, you take some scotch tape and put it on someone’s anus (anal hole) and remove it and you may or may not see a presence of eggs or the actual pinworms on the tape.
 < Strongyloids – Free living larvae penetrate the skin and can multiply outside or inside of the host (person infected). This worm can live up to and above 40 years, they tend to creep and run urticarial eruptions of the skin (especially around the anus and on the buttocks.
< Strongyloids – Free living larvae penetrate the skin and can multiply outside or inside of the host (person infected). This worm can live up to and above 40 years, they tend to creep and run urticarial eruptions of the skin (especially around the anus and on the buttocks.
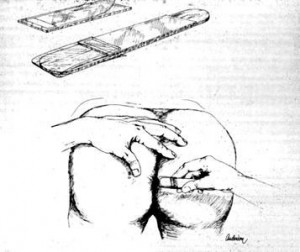 < Scotch tape method for pinworms
< Scotch tape method for pinworms
And then there were more graphic photos – but if you are really interested in seeing some of these photos, please let me know through comments or email and I will send you the lecture slides for you to see plus some related links so you know what you are looking at and can find some information about the worms/parasites.
NEXT!
It just gets better, so for lunch.. I had some chicken and veggies, a a yummy yogurt and granola but no.. no appetite anymore (my poor lunch just got to sit in the bag and not be eaten.
DIARRHOEA! Woohoo, no one is ever comfortable talking about this when it’s between yourself or the person(s) you may be talking too. No one likes to say “Well I had this bad bout of diarrhea yesterday, I just felt so bad and tired, but I think I got it all out of me!” or at least I don’t! But Diarrheal diseases are a HUGE problem in so many places and a leading cause of dehydration and death among children under 5 years of age! So here is my post on the fun stuff.
Definition – well I think we all know what diarrhoea is but just in case. It is defined as more than or equal to 3 loose/watery stools a day. Children between 6 months and 24 months are at the most risk of dangerous diarrhoea (especially if they are not breastfed and take cow’s milk or formula instead).
Causes – what are the main causes of diarrhea? (source: O’Ryan M et al. An update on management of severe acute infectious grastroenteritis in children. Expert Rev and Infect ther 2010; 8(6).671-682
| Watery Diarrhea | Bloody Diarrhea |
| Viruses | |
| Rotavirus | |
| Norovirus | |
| Bacteria | |
| ETEC, EPEC | Shigella spp. |
| Salmonella spp. | EHEC (STEC) |
| Shigella spp. | Salmonella spp. |
| Vibrio Cholerae | Campylobacter spp. |
| Parasites | |
| Cryptosporidium | Entamoeba histolytica |
Developments: Deaths in children have decreased by a fair amount but the numbers are still high! In 1979 the number of deaths of children from diarrhoea was 4.5 million, by 2002 it was only 1.6 million and by 2010 it was halved and only 0.8 million cases were reported. The areas in general with the highest reported numbers of mortality under 5 related to diarrhoeal diseases are India, and Africa.
Those at risk are of course infants with an incidence of 4.8 episodes per year, Children under 5 years with an incidence of 3.2 episodes a year and children in their 4th year with an incidence of 1.4 episodes per year. Malnourished children usually have more severe weight loss and longer duration of the bout of diarrhea. Infants usually have bouts of about or less than 6 months (especially when they are not breastfed. The hazard ratio for death of non-breastfed infants is 8.96!
What is dangerous diarrhoea? What makes it so dangerous? – it isn’t just uncomfortable.
- Risks associated and directly related to diarrhoea are dangerous dehydration! – with the loss of water from your body, you risk dehydration but with diarrhoea you also have a net loss of salts/electrolytes (K+ , Na+ and Zn++). There is also a loss of nutrients leading malnutrition or further malnutrition, typically with a decrease in appetite, depending on the victim.
Prevention – some very easy and simple things we and everyone can do to decrease the risk of diarrhoea for ourselves, themselves as well as for our or their children and future children.
- Breastfeeding during the first ½ year
- When women don’t exclusively breast feed their child in the first half year, mortality by diarrhoea increases by about 10.5 times! That is actually a lot! Such a simple thing can change so much. Some mothers have medical problems or issues that reduce their ability to breast feed their child for this long, if at all. Not breast feeding at all increases the incidence of diarrhoea by … guess?
- A whopping 165% !!! holy moly that is a big increase in mortality rate
- Continued breast feeding 6-23 months
- Continuing breast feeding as long as you can after 6 months helps decrease risks of diarrhoea. If no breast feeding after 6 months the risk is increased by 2.8 times (which is quite a bit still)
- Hand washing with soap
- Washing your hands after using the washroom, after being in pubic places, being near unwashed foods or tools, etc can decrease the risk by 31 – 48% because you kill the viruses and bacteria that may cause diarrhoea.
- Improved household water storage and treatment
- Water is a big thing, sanitation is a big thing. Who has heard and been reminded that when you travel to Mexico on your vacation – don’t drink the tap water! Don’t drink the ice from local lower end restaurants. The locals may be used to it, they can drink the water from the taps, but we are not used to it. We treat our water differently, and we are used to that. Traveller’s diarrhoea is a big thing that happens to so many people just from eating local foods without washing them or from drinking water from the tap that has not been treated thoroughly like our water is usually. So many bacteria, viruses and parasites all live in the water sources in developing countries, and without proper sanitation, extra steps need to be taken to ensure that the water is safe for you to drink.
- ORS – reduces diarrhoea mortality by 69% with current coverage or 93% if there is 100% coverage
- Zinc supplements
- Zinc for the treatment of diarrhoea reduces diarrhoea mortality by 23% – these are easily found in any supermarket or pharmacy that you can purchase before your trip. They even come in tasty chewable tablets!
- Rota Virus Vaccination! Which really should be part of the vaccination programs in high prevalence areas in my opinion
- When women don’t exclusively breast feed their child in the first half year, mortality by diarrhoea increases by about 10.5 times! That is actually a lot! Such a simple thing can change so much. Some mothers have medical problems or issues that reduce their ability to breast feed their child for this long, if at all. Not breast feeding at all increases the incidence of diarrhoea by … guess?
Treatment – very dependent on the severity of the diarrhoeal disease. For right now we are going to talk about treatment when severe dehydration is diagnosed. To treat dehydration you don’t just get the child or adult to drink a ton of water and overwhelm the system and kidneys, water isn’t the only thing missing. Electrolytes! They are very important and can be replenished through Oral Rehydration solutions (ORS). The ORS compounds offered by WHO and UNICEF include sodium chloride, potassium chloride, glucose, anhydrous and trisodium citrate dihydrate. All this together has an osmolality of 245 mmol/L. The newest formula of ORS solution with reduced levels of glucose and salt shortens the quantity and duration of diarrhoea and the need for unscheduled intravenous fluids. Though these are very effective, they are also very dangerous when they aren’t given in appropriate amounts at the right times. Initial rate of rehydration is by weight and always, ALWAYS, IF TOLERATED – sometimes a lower amount may need to be used so that the body will absorb it properly. Some examples of rate of rehydration are:
| Usual Weight | Encourage patients to drink at this rate: |
| 5 kg | 150 milliliters per hour if tolerated |
| 15 kg | 450 milliliters per hour if tolerated |
| 20 kg | 600 milliliters per hour if tolerated |
| 40 kg | 1,200 milliliters per hour if tolerated |
| 80 kg | 2,400 milliliters per hour if tolerated |
| 100 kg | 3,000 milliliters per hour if tolerated |
Zinc supplementation can help. The effects of Zinc supplementation help to decrease morbidity related to diarrheal infections. Zinc acts to accelerate the regeneration of mucosa, which in turn increase the number and level of brush-border enzymes. Zinc can also help with catch-growth by increasing IGF-1 (insulin-like growth factor-1) in children with stunted growth from malnutrition associated with diarrhoea. Zinc supplementation is usually given in 10-20 mg doses per day for 10-14 days to help lower the incidence of diarrhoea in the follow 2-3 months. WHO recommends that children under the age of 6 months should have this supplementation so that they decrease the initial risk of diarrhoea occurring.
Approach to diarrhoea.. 3 steps to know and use!
- Assess child with diarrhoea – assess the degree of dehydration [ask for symptoms and look for signs indicating other problems]
- Treat child with diarrhoea – select treatment and treat appropriately for degree of dehydration [treat for any other problems]
- Advise family members about home treatment of diarrhoea – counsel mother or care taker [teach mother or care taker to give ORS and zinc supplementation. Explain good food choices with examples, inform, educate and try to get mother to include breastfeeding]
The plan
Treat diarrhoea at home – counselling is very important when it comes to treating at home. The caretaker or parent (mother) needs to be educated and informed on the 4 rules of home treatment associated with diarrhoea:
- Give extra fluid (as much as the child will take) – never force it down their throat
- Breastfeed frequently and for longer at each feed
- If the child is exclusively breastfed, give ORS or clean water in addition to breastmilk
- If the child is not eclusively breastfed, give one or more of the following: ORS solution, food-based fluids (such as soup, rice, water, and yogurt drinks) or clean water.
- Teach the mother how to mix and give ORS safely and according to the weight of the child. Give the mother 2 packets of ORS to use at home
- Show the mother how much fluid to give in addition to the usual fluid intake
- Up to 2 years – 100 to 200 ml after each loose stool and between them
- Tell the mother to give frequent small sips from a cup.
- If vomiting occurs then wait 10 minutes then continue very slowly to reduce the risk of vomiting
- Continue extra fluid until the diarrhoea stops
- Five zinc supplements
- Inform mother on how much zinc to give and safety involved
- Up to 6 months – ½ tablet per day for 14 days
- 6 months and older – 1 tablet per day for 14 days
- Show the mother how to give the supplements to the child
- Inform mother on how much zinc to give and safety involved
But everyone has a PLAN B – just in case the above isn’t the best option
- Plan B: Treat some dehydration with ORS
- Give in clinic recommended amounts of ORS over a 4-hour period
- Determine amount of ORS to give during the first 4 hours
- Use the child’s age if you do not know the weight – amount is approx. 75 times their weight in kg.
And of course – there is a plan C for severe dehydration – treat quickly! (there are forms and instructions available for cases like this)
Wasn’t that fun 😛 I went a little information crazy on this one but I thought it was pretty interesting! plus.. the more you know the more it all makes sense and all that jazz, so I hope you learnt something from this too!