Schistosomiasis – fancy name for worms you get from walking around in freshwater.
This disease is really an important poverty related disease.
- Intensive utilisation of limited water resources – leading to an increase in schistosomiasis
- Water resource development such as dams and irrigation – lead to an increase in schistosomiasis
- Low mortality but high morbidity
Like I said, schistosomiasis is another name for worms but these worms come from an intermediate host of fresh water snails (can be various species of snails) and they tend to live in the mesenteric blood vessels or veins around the urinary tract for up to 30 years! Yummy!
There are 3 main types
- Japonicum – intestinal
- Mansoni – intestinal
- Symptoms include – the feeling of having to urinate frequently and blood in the urine
- Haematobium – urogenital
- Cause hematuria and bladder wall inflammation once the eggs are deposited (often in large clusters) in the urinary bladder or genital organs
Diagnosis can be pretty simple actually – check the colour of the urine, typically with schistosomiasis in the urine you see blood present. You can use micro-haematuria (dip sticks) to test as well then use Filtration and microscopy to count the presence of eggs per 10 ml of urine. (I learnt how to do this all in the microscopy lab practical session we had and there are actually a few ways you can filter the urine to find and count the number of eggs present). For diagnosis of the intestinal (S.Mansoni) worms you can microscopy for eggs within the stool, look for parasite DNA in the stool and clinically examine for liver and spleen enlargement. If the resources are available you can also do an ultrasound for detection of schistosomiases related morbidity within the abdomen area.
With intestinal schistosomiasis approximately 50% of the eggs will be trapped in the liver tissue or the tissue in the intestinal walls, this can lead to hepatosplenomegaly (the enlargement of the liver and spleen – giving a swollen belly look) and can lead to periportal fibrosis and/or portal hypertension.
What about Treatment? – drugs! To be specific… Praziquantel. This is really the only drug that is generally available in the areas that need it, but it also effective against all species of schistosomiasis and effective against adult worms and eggs. It is given in a single dose and can be given to women who are pregnant (which is really awesome).
- General strategies for the control of schistosomiasis include:
- Treatment of diagnosed positive cases in low endemic areas
- Mass drug administration (MDA)
- Mass treatment of school-aged children in moderate endemic areas
- Mass treatment of communities in high-risk/high-prevalence areas
After some discussion on Schistosomiasis we talked about the strategies for control of this parasite. As you see above one of the main strategies is MDA. I’ll give you a brief run down here on what MDA is and what would be involved
- MDA includes:
- A administration of drugs to whole populations irrespective of disease
- Often provided for free in order to reach all sub-populations, including the more vulnerable groups (dependent on prevalence of disease and population involved
- Target is usually all patrons aged 5 and older
- In areas of high co-prevalence of parasites, diseases and bacteria (sub-Saharan Africa), MDA includes a tablet cocktail of drugs
- Covering:
- Lymphatic filariasis
- Schistosomiasis
- Ascariasis
- Trichuriasis
- Hookworms
- Onchocericiasis
- Common drug cocktail used:
- Albendazole
- Ivermetin
- Praziquantel
- Covering:
Why use MDA?
- It has been shown to be effective in reducing individual parasite worm loads as well as reducing the number of new infections in a population or area
- The new overall aim of MDA however is to reach a complete elimination of specific parasitic infections (such as lymphatic filariasis and schistosomiasis)
Criteria for elimination of a parasitic infection
- To reach elimination, annual drug coverage rates in the rage of 65%-90% are required for approximately 4-6 years (which means 4-6 rounds of MDA)
- In these programmes, the combination of drugs id administered to all individuals in the target population once or twice annually for a 4-6 year period
- In order to reach this target however, a very high drug intake rate would be required.
Coffee break! Woohoo! There goes another 6$ for a delicious Cappuccino, totally worth it though. I don’t know if any of you have had coffee in Europe but it is friggen delicious. I don’t know what we do in Canada that makes it so … bitter? But I drink coffee here black or with a little milk and it is sweet and smooth but if I go to Starbucks or Tim Hortons and get a black coffee or Americano, it always tastes so metallic or bitter and needs some milk and maybe a sweetener of some sort.
Lymphatic Filariasis – because I was talking about it above I should probably fill you guys in on what this is and why it’s being talked about!
To understand lymphatic filriasis, one must understand the circle of life
Oh, wait.. that’s not right
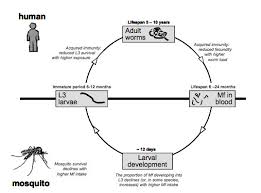
So as you can see (well you can’t because I can’t expand photos without making them blurry for some reason but pretend you can see….), starting with a mosquito landing and sucking someone’s blood is a microfilariae (mf) ingested into the mosquito where larval development occurs. This development allows for the larvae to become infective to humans. Once they are at this point and a mosquito lands on another human the larvae are deposited and then penetrate the skin. Once in the skin the larvae migrate to the lymphatic system and mature into adult worms. Then the adult worms (female and male), find each other and together and after a glass of wine, they produce the microfilariae (mf) which migrate to the blood stream, and there you have a circle because what happens to the blood? It gets sucked up by a damn mosquito!
- In the microscopy lab we got to look at the female, male and microfilariae. They were actually quite interesting.
Symptoms and ‘clinical manifestations’ (which a large portion of infected cases do not show any obvious clinical manifestations) of this parasite infecting a human include:
- Hydrocele (swelling of the scrotum in males) – ouch + graphic photos – if you are a male reading this, I suggest not googling these photos. This can also happen (similarly) in women with an enlargement of external genitalia – again I suggest not googling these photos because I got to look at this and it was not enjoyable
- Estimated in 25 million cases
- Lymphoedema/Elephantiasis of the leg (can occur in other areas of the body – rare)
- Estimated 15 million cases
- Acute adenolymphagitis
In filariasis endemic areas, typically there are 3 groups of individuals seen:
- Infected but free of overt disease
- Presence of adult worms and may or may not have microfilariae present
- Person(s) with one or more chronic manifestations
- May or may not have presence of either adult or microfilariae
- No sign of infection or disease
Interestingly enough, uninfected individuals have to receive a large number of infective bites before infection will occur. There is a very low risk of infection among migrants from non-endemic countries.
So to diagnose this lovely parasite, well actually, individual diagnosis is not of much importance. “But why? That just sounds stupid..” – Diagnostic tools play an important role when mapping the geographical distribution of infection – good for implementation of control programs AND when evaluating the outcome of a control program
Managing of the clinical manifestations
- Medication is given that is directed to the adult or the mf but this medication has little to no effect on any of the chronic manifestations (other management is needed)
- Hydrocele
- Hydrocelectomy
- Lymphoedema/Elephantiasis
- Improved personal hygiene
- Regular exercise of affected limb
- Raising affected limb at night (although not a sound solution..)
- Massage
- Bandaging (if done by a professional – otherwise can cause other complications)
And again we are brought back to MDA!
WHO recommends 3 things and that these should be offered once yearly for 4 to 6 years:
- Diethylcarbamazine (tablet 6mg/kg of bodyweight) + albendazole (400 mg)
- Diethylcarbamazine-medicated cooking salt
- Ivermectin (200 micrograms/kg bodyweight) + albendazole (400 mg)
And that’s a wrap!