When facing sickness, some stay home to rest and recover where others will seek treatments to accelerate the recovery period from their doctors. When treating illnesses, such as pneumonia, with antibiotics, a possibility for the pathogen (viruses or bacterium) to develop immunity to these antibiotics increases, posing a great threat to human health across the world. The inability to treat treatable illnesses with antibiotics leaves individuals in pain, agony, or ultimately death. In the United States alone, each year approximately 2 million people face antibiotic-resistance infections and of these 2 million cases, approximately 23,000 result in death.
Individuals throughout the world require and depend on antibiotics for various infections and are usually unable to heal themselves alone, susceptible to complications from the infections, and are commonly referred to as the at-risk population. Such individuals include elderly, children, pregnant women, and people with weakened immune systems, however healthy populations are additionally at risk. For example, 2 in every 100 people carry methicillin-resistant Staphylococcus aureus (MRSA) which is a skin-dwelling bacterium resistant to many antibiotics. When hospitalised, it is not uncommon for healthy patients to contract MRSA from MRSA-infected patients in the same facility. For protection of those at-risk and ourselves, antibiotic resistance must be studied in-depth for determination of mechanisms to potentially block formation of such bacterium.
Video 1: What causes antibiotic resistance? TED-Ed YouTube Channel.
What is antibiotic resistance?
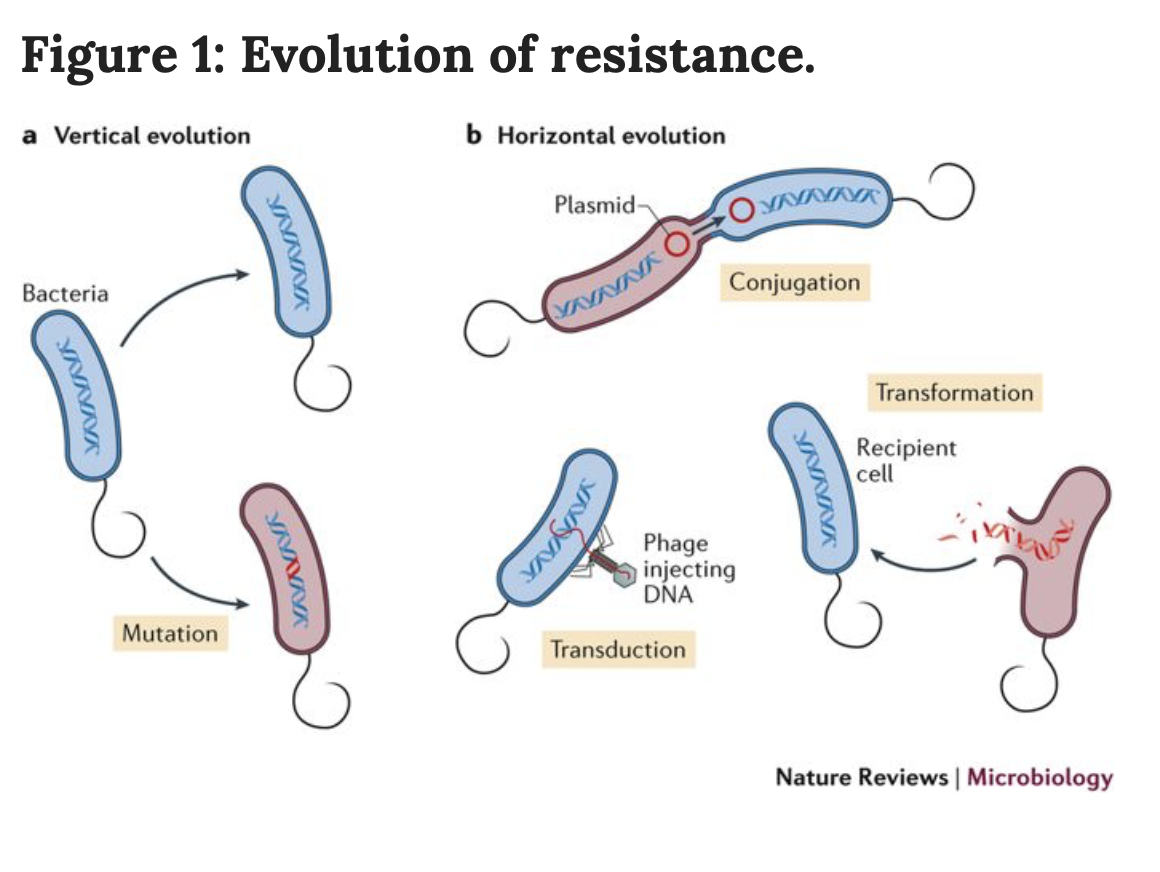
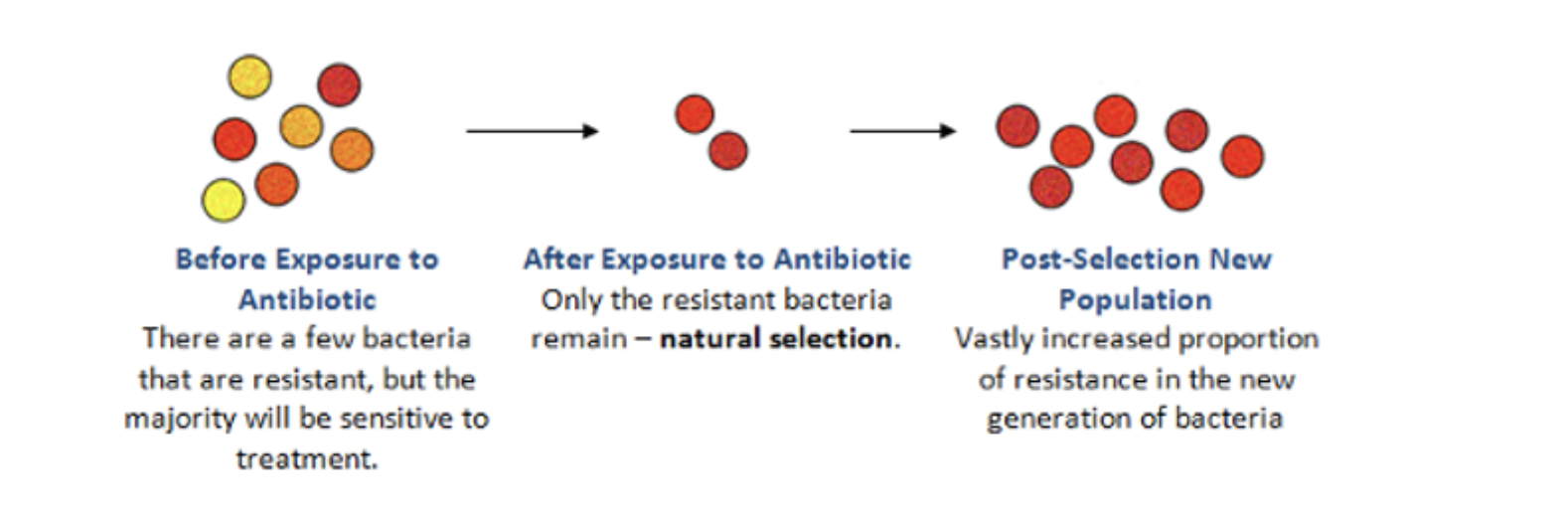
When a species is faced with environmental stress, the individuals possessing certain characteristics are able to survive. Additionally, there is a term called ‘biological fitness’ which is an individual’s ability to successfully produce offspring in the natural selection mechanism. When a bacterium survives the environmental stress caused by the antibiotics, this bacterium can go on to produce offspring that are copies of itself. These bacterium will all be resistant to the antibiotic from the initial exposure and can go on to create a resistant colony. Additionally, bacterium can quire antibiotic resistance through complex genetics involving the transfer of genetic material from one cell to another or through mutations. Antibiotic resistance is not only a threat to at-risk populations but to all populations and if not researched can potentially lead to emergence of larger problems. For example, as antibiotic resistance becomes increasingly common, as will the emergence of superbugs which are bacterium that carry resistance genes for multiple antibiotics and require harmful super-antibiotics with severe side effects for their treatment.
Figure 1. Figure displaying genetic methods for acquisition of resistance genes into the genome (library of DNA in the cell). Source: Nature Reviews Microbiology
Figure 2. Basic figure demonstrating the mode of antibiotic resistance in a general summary. Source: Reading Borough Council
Video 2: The Antibiotic Apocalypse Explained Kurzgesagt – In a Nutshell YouTube Channel.
How are we approaching a solution for antibiotic resistance?
Researchers have been attempting to find a solution for antibiotic resistance and a recent study has found possible treatments for the restriction or reversal of antibiotic resistance development. One treatment involves the combination of drugs that interact and have varying effects has been used to slow or reverse the progress of antibiotic resistance. Additionally, a treatment involving the use of drugs with effects that fluctuate during the growth of resistance can be used to rid of resistant bacteria. Finally, a treatment involving the use of one compound to increase a bacterium’s sensitivity to another compound was used. The above described methods provide promising treatments that, once further investigated, can potentially provide clinical medicine ways to rid of antibiotic resistant bacterium.
Video 3: Rise of the Superbugs It’s Okay to Be Smart YouTube Channel.
Antibiotic resistance is prevalent across the globe and poses a threat for at-risk populations as well as for sudden susceptibility from hospitalisation. With further development of clinical treatments for these resistant bacterium, at-risk populations can go through their lives with less worry. Further research into the newfound treatments can potentially discover a solution for eradication of superbugs and thereby potential pandemics. Additionally, hospital patients can be at ease knowing effective, less harmful treatments are available for resistant bacterium possibly acquired during stays. Because of the prevalence antibiotic resistant bacteria pose in society, these newfound findings provide hope for clinical medicine across the world and steps forward towards a solution for a global problem. The next time you go to the doctor for a viral or bacterial infection, think about antibiotic resistance and the true need for antibiotics to recover versus antibiotics to recover rapidly.
-Vanessa Niedzielski

2 responses to “Reversing antibiotic resistance: the enemy of society”