What is Spina Bifida?
I believe some of you may have heard about neurodevelopment disorder like hydrocephaly. What about the disorder strong related to hydrocephaly – Spina Bifida. Literally speaking, Spina Bifida means the spine split into two. It happens within the first four weeks the fetus in the uterus. Due to the spinal column is not fully closed, the spinal cord inside is not covered and even exposed and protruded out of the spinal column. There are about 120 children born with Spina Bifida each year in Canada, and 90% of them can survive and become adults.
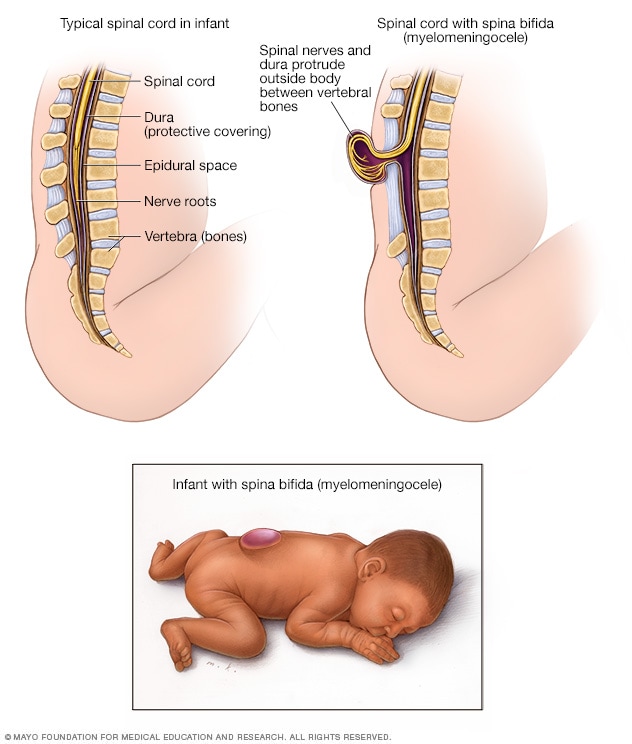
Image Credit: Mayo Clinic

Video Credit: The Spina Bifida Resource Network
Spina Bifida has more than one type. What do they look like?
There are two main types of SB, Spina Bifida Occulta (SBO) and Spina Bifida Myelomeningocele (SBM).
SBO is the mildest case which does not show any symptoms of the condition. The defect is hidden under the skin, and the spinal nerves are not involved in the defect. This type of defect may be noticed early in life if there is an abnormal tuft or clump of hair, or small dimple or birthmark on the skin at the site where the spine is not formed correctly.
However, SBM, also known as open SB, is the most severe form which needs to be treated with surgical treatment as early as possible. The membrane and spinal nerves push through the opening between spinal column gap at birth, forming a sac on the baby’s back. In this situation, the spinal cord is exposed, causing partial or complete paralysis of the body.
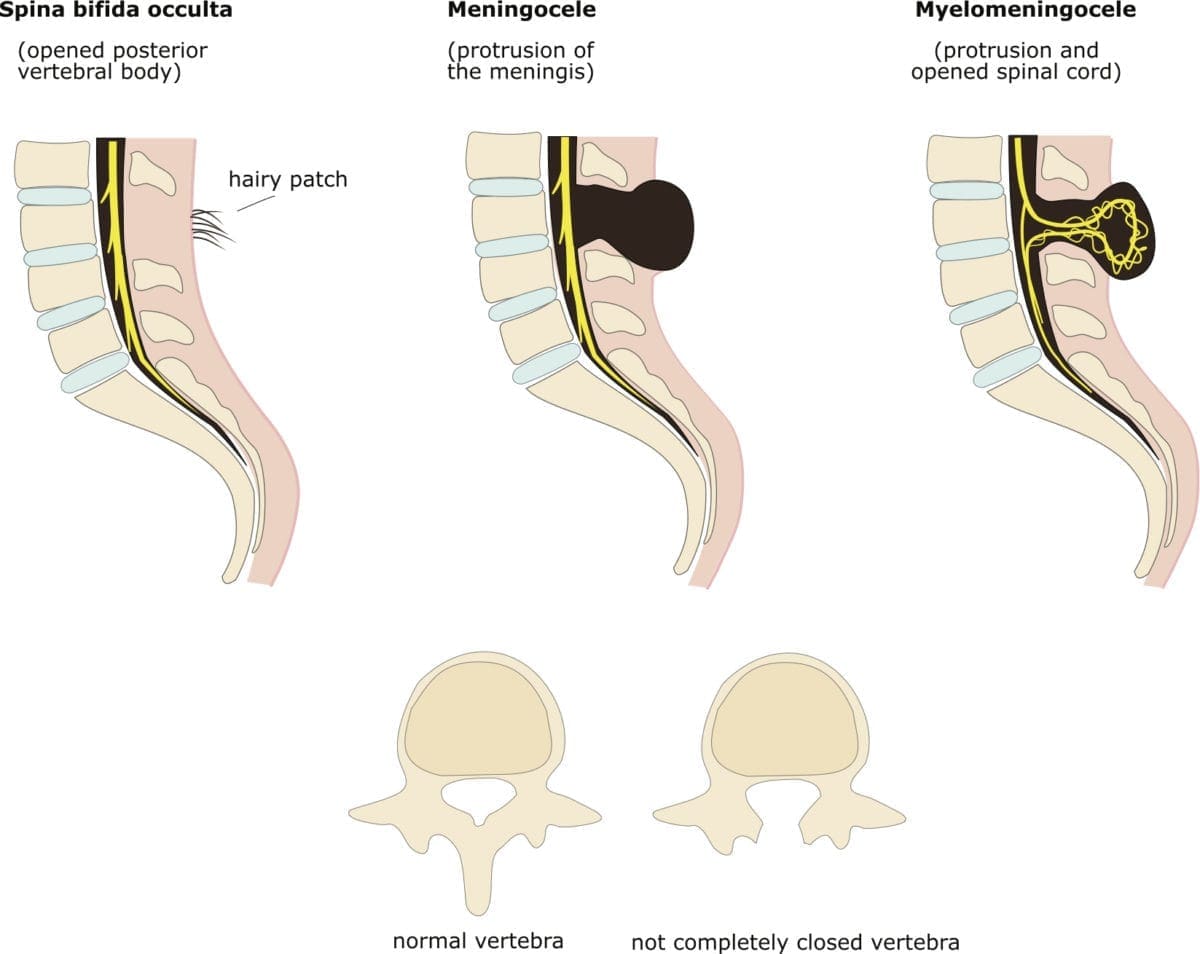
Image Credit: familydoctor.org
Causes & Risk Factors
The specific reason for spina bifida is still not clear nowadays. It shows to result from a combination of genetic and environmental risk factors, such as family history of neural tube defects and folate deficiency during pregnancy.
Then how should we prevent this disorder? Scientists find out that folate plays a significant role in SB prevention. Low levels of the vitamin folic acid during pregnancy are linked to SB.
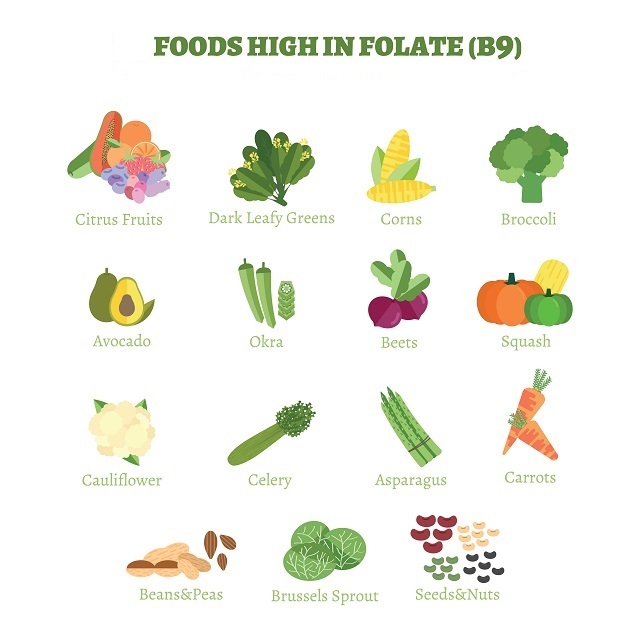
Image Credit: Babyment
how to treat the disorder?
Treatments for SB also depends on the type of SB. Children with SBO typically do not have any symptoms or complications, only routine pediatric care is needed. However, the child with SBM needs to be treated with surgery. The research finds out that fetal surgery can be an effective management strategy for SBM patients, resulting in a significant benefit to these patients, typically in improving motor function.
Another study investigates the neurodevelopment outcomes of preschool children with SBM treated with myelomeningocele closure. They found children who have undergone fetal myelomeningocele closure have average preschool neurodevelopment scores.
– Elaine Yuling Chen
