Many people have a friend or family member who is afflicted by Parkinson’s Disease, a long-term degenerative disease affecting the brain’s central nervous system. Seemingly unrelated, many people also have removed their appendix, a small finger-like length of intestine that is widely removed due to appendicitis. Perhaps somewhat unexpectedly, a recent study analyzing more than 1 million people in Sweden has concluded that an appendix removal done decades ago may reduce the chances of developing Parkinson’s Disease (PD).
Scientists speculate that the removal of the appendix affects the development of an abnormally formed protein, named α-synuclein (alpha-synuclein), which is present in PD patients.
What Is Parkinson’s Disease?
Parkinson’s Disease is a genetic neurological (brain) disorder that can have significant impact on the physical and mental state of patients, with more than 55,000 Canadians diagnosed with PD. The onset of PD is slow, often alongside symptoms such as hand tremors and body stiffness.
Parkinson’s encompasses a wide subset of symptoms and related complications: restricting the movement of a patient gradually, eventually initiating other symptoms such as difficulty speaking, loss of coordination, and development of depression.
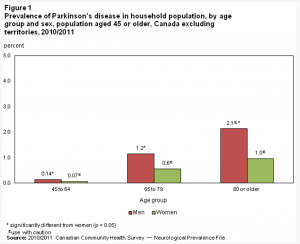
Prevalence of Parkinson’s disease in household population, by age group and sex, population aged 45 or older, Canada excluding territories, 2010/2011 Source: StatCan
Presence of α-synuclein In PD Patients
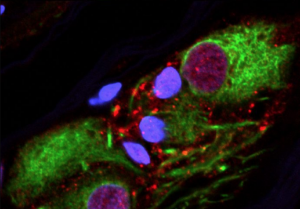
A protein called α-synuclein, in its misfolded (mutated) form, is fairly abundant in the appendix of both healthy people and PD patients. The mutated version of α-synuclein has the same structure as the version of α-synuclein that is found in the brains of patients afflicted by PD, which scientists have suggested causes PD by damaging the brain cells which control bodily movement.
α-synuclein tends to travel from the appendix, leading scientists to investigate whether the protein present in the appendix is the same as the protein in the brain of PD patients.
Study on More than 1 Million Swedes Found…
Knowing this information about α-synuclein, Viviane Labrie (the first author of the study) and her team at the Van Andel Research Institute in Michigan analyzed 1.6 million Swedish medical records to find that appendix removal showed almost a 20% decrease in chances of developing PD.
The data analysis also showed that an appendix removal also delays the diagnosis of PD for the people in the data set who did go on to develop PD for more than 3 years.
Why Is This Important?
Parkinson’s Disease is not only a devastating and debilitating disorder, but also it is increasingly common as the general population begins to age. In recent years, PD is affecting more than 60,000 people each year in the United States. As PD is the second most common neurodegenerative (brain disorder) disease in Canada, it is with hope that these findings will inspire investigations into the pursuit of a treatment for Parkinson’s Disease.
See below for a video posted by Parkinson Society of BC, showcasing a young patient and her goals despite her disorder.
An instalment of Parkinson Society of BC’s This Is Parkinson’s Disease campaign, sharing Hilary’s story: a real-life British Columbian living with PD.
Source: Parkinson Society of BC
-Allison Chiang