Ray Cam Community Clinic stirred in me a great interest in the low socioeconomic population. Currently 1 in 7 Canadians live in poverty.1 Low income populations tend to experience greater health inequities such as poor access to health services, systemic health conditions (high blood pressure, obesity), and poor oral health.1 The low socioeconomic population face the double burden of having the highest level of oral health problems and the greatest barrier to oral health care.2,3 Cost of dental treatment remains to be a deterring factor for those struggling financially.1 Although, the Canada Health Act states “continued access to quality health care without financial or other barriers will be critical to maintaining and improving the health and well-being of Canadian”, there is a absence of a policy attempting to achieve “continued access without financial or other barriers” enacted for oral health care.2,3
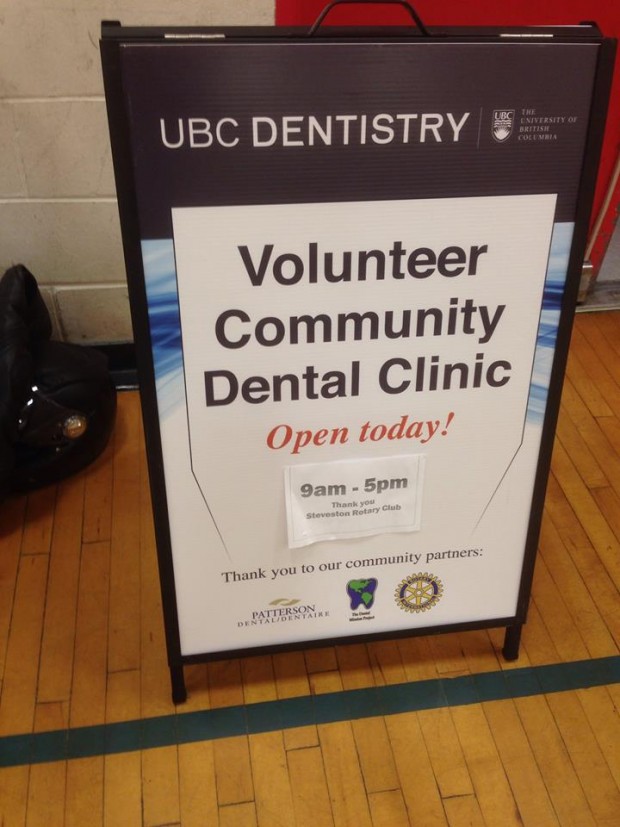
The clinic was held in Ray Cam Community Centre, situated in Downtown Eastside in Vancouver, a region known as Canada’s poorest postal code. Many individuals who sought care from the clinic were predominantly elderly individuals of Chinese descent and had not seen a dental professional for 10 to 15 years. Working along side an experienced registered dental hygienist and two other dental hygiene students we managed to provide dental hygiene services to more than 30 individuals. This was also my first exposure to an individual with severe chronic periodontitis and an “wall to wall” calculus. This community initiative allowed me to use my the talents, skills, and knowledge I have acquired from my undergrad career to serve a marginalized population.
- The Canadian Academy of Health Sciences. Improving Access To Oral Health Care For Vulnerable People Living In Canada. 2014
- Provincial Health Services Authority. Towards reducing health inequities: a health system approach to chronic disease prevention. Vancouver (BC): Population & Public Health, Provincial Health Services Authority; 2011.
- Health Officers Council of BC. Health inequities in British Columbia: discussion paper. Vancouver (BC): Public Health Association of BC; 2008.