Seasons greetings to all.
An Interesting Case
This year I decided to pursue a complaint against a practitioner with the College of Registered Nurses of British Columbia (CRNBC) for a nurse who was using their Registered Nurse (RN) title to market their own private Therapeutic Touch (TT) business. To those outside of the nursing profession this might seem a little confusing, but in other countries where I have worked as a nurse it is an established professional principle that you do not use your professional qualifications/status to promote your own for-profit activities outside of your role as an RN. The reasons for this would seem fairly self-evident. For example adding RN to your name gives you some professional credibility and it would be disingenuous to use it for personal gain, such as by selling something (be it real estate, car parts, vitamins or personal life-style counselling). The CRNBC has established standards governing use of title, and has even produced guidance for practitioners with a case example to explain this. See: Can she Use her Title? where they note that having “RN” after your name may be seen as “…important in gaining the public trust and selling more product.”
Indeed, it was this very article that incited me to make the complaint as a test case, as I came across a TT practitioners website where the title of RN was explicitly used next to the practitioners name. I used the exact format and language in the guidance for the complaint and cited the relevant “Use of Professional Titles” standard and College Bylaws (sections 4 & 8) in the complaint, and asked that the CRNBC to ask the practitioner not to use the RN title on their website. I had been in contact with this individual on other occasions and suggested that the use of RN was inappropriate to endorse this business activity. Unfortunately, I had a completely negative response, so a simple complaint to the CRNBC on appropriate use of title seemed an appropriate next step.
At this stage it is probably worth a quick recap on what the professional regulators function is. Basically, the regulation of nurses includes licensing, the creation of professional standards, enforcement of those standards, disciplinary measures and nursing education approval. Overall, the key principles that underpin the statutory professional regulation of nursing may be considered as:
(a) maintaining the safety and quality of the care that patients receive from health professionals;
(b) sustaining, improving and ensuring the professional standards of health professionals and identifying and addressing poor practice or bad behaviour;
(c) providing systems and legislation that sustain the confidence of both the public and the healthcare professions through demonstrable impartiality; and
(d) ensuring that the integrity of health professionals is sufficiently flexible to effectively meet the different health needs of the public and healthcare approaches can adapt to future changes and demands (Hewitt 2007; ICN 2014; Walsh 2012; WHO 2002).
To ensure that regulatory standards are effective, the regulatory process itself also needs to be seen as impartial and independent from the government, the professionals themselves, employers, educators and all the other interest groups involved in healthcare (Hewitt 2007). I.e. the CRNBC should represent the interests of the public at large rather than the profession or government (this is an important point, which we will come back to). So, one would think that in terms of public protection this complaint would represent a fairly straightforward case of inappropriate use of title to support a commercial enterprise.
Another consideration here is that in this case the title was being used to help market a completely unscientific, non-evidence based and “unverifiable” practice (as indicated by the CRNBC’s own Bylaws, 2012; Section 8.04). We have discussed the merits of TT on this blog before, and it is of course, pure magic in the terms it is portrayed (remote healing using undetectable energies) with no-scientific evidence to support efficacy. A 1999 review of the physics of complementary therapies states that the existence of a “bio-field” or “bio-energetic field” directly contradicts principles of physics, chemistry, and biology (Stenger, 1999). A recent Cochrane systematic review found “no robust evidence that TT promotes healing of acute wounds (O’Mathúna et al, 2012). The American Cancer Society stated in 1999, “Available scientific evidence does not support any claims that TT can cure cancer or other diseases” (AMA, 2012). Lastly we have the youngest person ever to get a paper published in the Journal of the American Medical Association ( the nine year old Emily Rosa) presenting a study that debunked the claims of TT practitioners in a simple study where twenty-one practitioners of therapeutic touch failed to detect her aura (Rosa et al, 2009). TT is then, complete mystical woo-woo, and fails to meet any test of scientific credibility in that 1) the underpinning theory is tautological nonsense, and b) practitioners can demonstrate no efficacy better than placebo. No respected university will touch TT practical training with a barge pole. Nevertheless, we should note it is a highly profitable enterprise (the overheads are minimal) and many nurses do support it. The professional regulator would seem to have some responsibility to ensure practitioners are using evidence-based practices, and TT (based on current evidence) clearly falls outside that scope.
The Outcome
Anyhow, in the end the CRNBC disposition on this case earlier this year sided with the practitioner, and that they were perfectly entitled to use their RN credentials to market their TT business as they found that:
a) the regulations are not intended to apply to RNs providing education services. The CRNBC regarded this registrant as providing an educational service, as the website identified was aimed at a TT consultation service.In other words they viewed an educational service as not being a product (even though it was a commercial, for-profit enterprise)!
b) Alternative and complementary therapies are considered within the realm of holistic nursing.
Given the CRNBC’s position on CAM in general, I was not unduly surprised with this outcome, but am concerned this represents a particularly troubling precedent as point a) represents a very narrow view of what a commercial product is, and also implies you can sell health education on anything (whether good or bad) and simply tag your RN credential to your marketing materials. Point b) is even more worrying as it represents an “anything goes” approach to the regulation of RN practice (as long as you don’t physically hurt anyone; it’s all good). This completely ignores the responsibility to make sure practitioners don’t financially or emotionally exploit the public, and tarnish the reputation and credibility of the nursing profession.
Let’s examine a comparable example. If I want to promote my business as a tarot or astrology based health practitioner, and make good money selling my advice and education to the public who believe in this. Then I can tag on my RN credential to give it an air of professional respectability, better market my magical consultation services and improve my profits. Its all good!
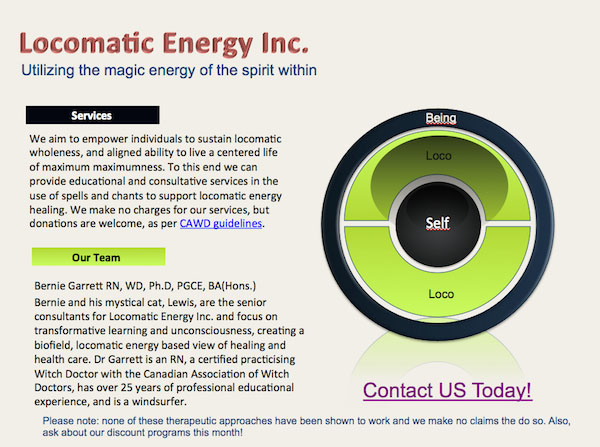
I can’t help but ask; how does this approach protect the public rather than the profession? The finding here does nothing to protect the public from exploitation, and seems to give carte blanche for RNs to practice magic. To illustrate this, I have just acquired a practising Witchdoctor (WD) certification from the Canadian Association of Witch Doctors (it was a tough program, and examination I can tell you)! So, with my new magical powers, apparently using my title in the following advertisement is perfectly within my scope as an RN:
Click here to see the full size Locomatic Energy Inc Advert
This advert covers the same ground as the website I originally made my original complaint against (well, apart from the cat, services being free and the windsurfing). The use of the RN title to support this sort of activity is clearly nonsense, and to be frank, supporting it is a travesty of regulatory practice and represents an example of where our professional regulatory body is failing miserably. Regulators traditionally err on the side of caution, remain impartial, and represent the public interest, not those of the professionals they regulate. In this case I would argue they clearly failed to meet their regulatory obligations in this respect.
Other nursing and health professional regulators I have observed seem to do a much better job in this area. The College and Association of Registered Nurses of Alberta (CARNA) Standards on CAM, 2011 notes:
“Registered nurses cannot use the title ‘RN’ or ‘NP’ in association with the endorsement or promotion of products or services. Endorsement of a product or service occurs when a nurse uses their credentials to lend credibility to a commercial product or service (CNO, 2009). The endorsement of a product or service without providing information about other options could mislead the public and may be considered a conflict of interest.”
Likewise the College of Nursing of Ontario, Professional Misconduct Regulations, 2014 states:
“It is not acceptable for a nurse to use her/his registration status to promote personal interests such as commercial products or services. Endorsement occurs when the nurse inappropriately uses her/his credentials to lend credibility to a commercial product, product line or service. The endorsement of a product line or service without providing information about other options has the potential to mislead the public and compromise trust.”
Both clearly indicate services (such as educational consultation) are to be treated the same as products in this respect. In the UK, The Nursing and Midwifery Council Code of Conduct 2014, is similarly clear, requiring practitioners to:
- not abuse your privileged position for your own ends.
- ensure that your professional judgement is not influenced by any commercial considerations.
- uphold the reputation of your profession at all times.
- ensure that the use of complementary or alternative therapies is safe and in the best interests of those in your care.
The College of Surgeons and Physicians of BC are also much clearer on how we should consider CAM in respect to public healthcare:
“Practitioners must not misrepresent the safety or efficacy of any therapy or procedure.”
“Complementary and alternative therapies differ from conventional medicines because they are generally unproven. When an alternative treatment undergoes rigorous testing, for example in a controlled and randomized trial, then the results dictate whether the alternative treatment becomes conventional treatment, whether the unorthodox becomes accepted, and whether the unproven becomes proven. Assertions, speculations, and testimonials do not substitute for scientific evidence.”
I did briefly pursue this CRNBC disposition on this case with the BC Health professional Review Board (HPRB), but have dropped it, as there is really nothing they can do in such a case as the HPRB are focused on interpretation of process and the law and are very unlikely to intervene in what they see as “professional jurisdiction” unless there is clearly evident harm arising. Astonishingly, it appears guidance published in CRNBC newsletters and advice has no real legal grounding anyhow, so can be completely different from interpretation of the actual standards by the disciplinary board. This doesn’t seem to reflect a well coordinated organization to me though. So, my next action is another formal approach to the CRNBC (I have raised this issue with them before) requesting they review their regulations and toughen them up in this respect.
Finally, although TT is generally harmless, we should be reminded these are serious concerns and not the trivial issues they are often taken as. Firstly, financially exploiting vulnerable people is a serious issue. Secondly, where the public are advised to consider alternatives to conventional evidence-based treatments, life-threatening results occur, as exemplified by the recent cases of the parents of two children with acute leukaemia seeking CAM remedies, and with people being advised to take homeopathic vaccines rather than actual vaccines. If we continue with this approach to regulation and CAM practices, and allow them to be marketed with implied professional support, sooner or later deaths or injury will result from people In BC choosing CAM over medical alternatives on the advice of a nurse using their professional title to support their CAM practice. Effective regulation can help prevent this.
So, are nurses in BC licensed to practice magic? What do you think…
Bernie
References
American Cancer Society (2012) Therapeutic Touch. Retrieved 20 October 2014.
Hewitt, P. 2007. Trust, Assurance and Safety – The Regulation of Health Professionals in the 21st Century. London: H.M. Stationary Office
International Council of Nurses (2014). Regulatory Board Governance Toolkit. http://www.nurse.or.jp/nursing/international/icn/report/pdf/2014m/04-04.pdf. Retrieved July 29, 2014.
O’Mathúna, D. N. P.; Ashford, R. L. (2012). O’Mathúna, Dónal P, ed. Cochrane Database of Systematic Reviews (Online) 6: CD002766
Rosa, Linda; Rosa, E; Sarner, L; Barrett, S (1998). “A Close Look at Therapeutic Touch”. JAMA 279 (13) 1005–10
Stenger, Victor (1999). “The Physics of ‘Alternative Medicine’ Bioenergetic Fields”. The Scientific Review of Alternative Medicine. 3(1) 79-84
Walsh, P. 2012. “Health Professional Regulation.” AvMA Medical and Legal Journal 18(3): 3–4.
World Health Organization (WHO). 2002. Nursing and Midwifery: a Guide to Professional Regulation. Cairo: WHO Publications Eastern Mediterranean Regional Office.
Other Relevant Sources
1. The CRNBC has a self-identified mandate to “protect the public through the regulation of registered nurses and nurse practitioners: https://www.crnbc.ca/crnbc/Pages/Default.aspx
2. Registrants are required to use their title(s) in ways that comply with the: CRNBC Standards of Practice. See: https://www.crnbc.ca/Standards/Lists/StandardResources/343AppropriateUseofTitlesPracStd.pdf
3. CRNBC October 2013 case study “Can she use her RN title?” which was subsequently amended – current version is at: https://crnbc.ca/Standards/resourcescasestudies/beinganurse/selfemployment/Pages/marketing.aspx .

 Follow
Follow