We are currently investigating the use of VR in a small number of individuals with chronic pain. Individuals with a diagnosed chronic pain condition have been recruited to the study.
Why the Research is being done?
There is potential that virtual reality may help patients with chronic pain manage their pain symptoms in their own homes. Currently there is limited evidence of the use of virtual immersive reality in people with chronic pain. The case series will investigate the use of VR in the home for 10 individuals with chronic pain. Adults with chronic pain will be invited to participate in the study. The VR intervention will be identical for each participant, and participants will be asked to use the VR therapy every other day with a time exposure of 30-40 minutes for a study period of 1 month. This will equate to 15-16 therapy sessions.
Our aim will be to undertake a preliminary exploratory study to examine the use of VR for patients living in the community with chronic pain. We are interested in exploring the use of VR in the home. As well, to explore if the VR results in any changes in the individuals pain experience. To undertake this small exploratory study we propose a prospective case series involving a small number of patients with chronic pain. This will be a small descriptive study which will track patients utilizing VR in their homes to explore the impact this may have on their pain experience. This will allow us to develop much needed knowledge with regard to the feasibility of using VR for individuals with a chronic pain condition.
What is Virtual Reality and How it Can Manage Chronic Pain?
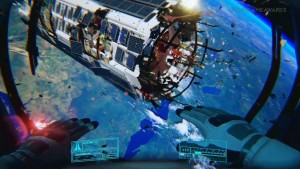
Virtual reality enables individuals to become immersed within computer generated three dimensional worlds and immersed within the virtual environment. The immersed individual is able to be an active participant of the computer generated 3D World.
These technologies have been shown to benefit individuals from a range of clinical settings such as patients with acute pain and burns injured patients. The immersive virtual reality is thought to reduce the chronic pain by changing the pain signals of the pain modulation system within the central nervous system by manipulating the descending pain signal pathways.
Data Collection
We are collecting data from participants which will allow us to measure the impact of VR on the individual’s pain experience, pain intensity and experience of immersion.
VR Intervention
The VR hardware will be identical for each VR subject, and consist of a PC running the VR application with an Oculus Rift 1100 FOV HMD. This new HMD was selected due to its light-weight, good resolution and FOV, and practical affordability for clinical use (SIAT has reviewed pre-release versions). The VR will be an exploratory virtual environment game designed for the Oculus Rift headset, to be selected from: http://en.wikipedia.org/wiki/List_of_games_with_Oculus_Rift_support
The VR Interventions will be: Commercially available VR game environments designed to provide an interactive journey, exploration or relaxing: Week 1: Orientation to VR using the Oculus Rift Tuscany VR demonstration, Phillip Schmidt’s Iceland environment, and The Senza Peso VR mini Opera. Week 2: Guided mediation, Over the Alps and The Wild Within and Sightline: The Chair. Week 3: Ocean Rift, Discovering Space & In Mind Week 4: Sub Nautica, Pneuma-Breath of Life, and Ether One.
Reference websites for the games used:
http://vergevr.com/creations/iceland
http://senzapeso.com/
https://share.oculus.com/app/discovering-space
http://www.thegallerygame.com
https://forums.oculus.com/viewtopic.php?f=42&t=15703
http://en.spaceengine.org/
http://guidedmeditationvr.com/
http://www.wilddivine.com/sun-realm/return-to-the-sun-realm-pc-download/
The intervention is being used for one month to enable customization to the therapy and record data over a long enough period of time to account for individual short-term changes in pain experience. Participants will be asked to use the VR therapy every other day with a time exposure of 30-40 minutes which will equate to 15-16 therapy sessions. In associated literature regarding hypnosis use for chronic pain it has been demonstrated that studies giving between 6-12 sessions can result in significant improvements in pain control and outcomes (Jensen 2014). Currently it is reasonable to compare hypnosis as similar to VR with regard to effects on pain, as it appears to alter the central processing and appraisal of pain in a similar manner. Hypnotherapy pain studies that used 4-6 sessions had less success. As well, time of exposure for the studies that had offered 8-12 sessions had lengths of exposure to hypnosis between 30-40 minutes and established positive results (Elkins, Johnson & Fischer 2012). Given these findings, an initial exposure to 15-16 therapeutic sessions would seem adequate to establish if any clinical effects of VR in chronic pain reduction are evident.

Instruments for Data Collection
To ensure the multi-dimensional aspects of chronic pain experienced by individuals are measured adequately, tools have been selected that will address different aspects of chronic pain and participant’s functional capacity. To measure the impact of VR on the participant’s pain intensity participants are rating and recording their pain intensity using a numerical pain rating immediately before the intervention, immediately after at 6 and 24 hours post-intervention. Given the persistent nature of chronic pain these measurement points will allow the capture of any residual therapeutic effects or trends following the intervention.
The brief pain inventory (BPI) and the self-complete Leeds assessment for neuropathic symptoms and signs (S-LANSS) will be used to capture detailed pain assessment data at the end of each week of therapy. Additionally, a VR immersion and presence questionnaire will be administered after the each weekly experimental VR period.
a) Demographic baseline health survey:
A short survey has been implemented at the start of the study by a research assistant (RA) to capture basic biographic information from participants (e.g., ethnicity, age, gender, level of education, prior VR and computer gaming experience, duration of pain, cause of chronic pain, current pharmacological management for pain).
b) Numerical rating scale (NRS):
The pain intensity numerical rating scale is being used to assess for any overall changes in pain intensity. This meets the IMMPACT group recommendations for using a global impression of change question, and as a visual analogue scale (e.g. a change of 6 to 3 is scored the same difference as a change of 5 to 2) and has been used as an interval level data tool with demonstrated validity and sensitivity to change (Breivik, Bjornsson, Skovlund 2000; Herr, Spratt, Mobily & Richardson 2004). In this study participants are required to self-complete the NRS scale at the start of the study as a baseline, before and immediately after treatment and 6 and 24 hours following VR exposure.
c) Brief pain inventory (BPI):
To gather structured descriptive data on changes in chronic pain the BPI is being used. The BPI has been used in numerous studies and has been used in several studies investigating pain (Cleeland 1994; Sawatzky, Slobogeam, Reilly, Chambers, Hol 2005; Stroud, Turner, Jensen, Cardenas 2006). It requires patients to rate their pain at the time of responding to the questionnaire (pain now), and also at its worst, least, and average over the previous week. The BPI uses questions of the degree to which pain interferes with mood, mobilizing and other physical activity. The shorter version has become the standard for use in clinical and research applications, and is typically what is referred to when the BPI is cited in research (Cleeland, Ryan 1994). Participants are required to self-complete the short-form BPI initially (as a baseline) and then weekly during the study.
d) The Neuropathic pain scale (NPS)
The NPS is being implemented as a baseline then weekly during the study to assess changes in neuropathic pain. The scale has been designed to measure pain qualities associated with neuropathic pain and treatment effects. The NPS is a quick to use self-report scale for measuring neuropathic pain, and consists of 12 distinct questions, which ask about the intensity and quality of the patients’ pain. In validation studies it has been found to have a good predictive power in discriminating between subgroups of patients with neuropathic pain (Bennett, Smith, Torrance & Potter 2005). It provides ordinal level data for descriptive and comparative analysis. A secure data collection file will also be provided to fill in the NPS scores, as with the BPI.
e) VR immersion questionnaire:
Each week following the VR interventions the questionnaire is being administered to the participants by the researchers. This has been developed as there were no suitable validated pre-existing tools. The questionnaire has been based on existing immersive theory and tools (Jennett, et al. 2008; Bowman & McMahan 2007; Lin, Duh, Abi-Rached, Parker, & Furness 2002) to explore both depth and breadth of immersive experience (Steuer, 1992; Nechvatal 2009). It uses closed questions on specific elements of VR and Likert scaled attitudinal questions to provide ordinal level data for analysis of the users perceptions of the level of immersion provided by the specific VR used.
Data Analysis
Due to the small numbers involved in this study descriptive statistics will be collated and presented, this will allow for a preliminary understanding with regard to the impact of VR on an individual’s pain experience. Descriptive statistics will allow for initial understanding to this new and novel therapy. A descriptive statistical analysis will be performed for face-value quantitative indicators of potential effects employing univariate descriptive statistics. Data will be analyzed for central tendency, dispersion (standard deviation, interquartile range), skewness and kurtosis using SPSS statistical analysis software to establish distribution and variance. Data will be explored for differences in the pain scales for the VR intervention at each time point to analyze for any indications of changes immediately following VR, 6 & 24 hours after exposure. Given the ordinal basis of the BPI, NPI and immersion scores, it is preferable to summarize the central tendency of responses by either median or the mode, with ‘spread’ measured by quartiles or percentiles (Jamieson 2004).
Knowledge Translation and Dissemination
This study supports a knowledge translation (KT) process designed to develop theory based on pre-existing lab-based innovation, and further define the practical determinants, implementation and uptake considerations for VR use in wider practice. The results of this small case series will be published in relevant clinical journals and presented at relevant clinical/scientific conferences e.g. International Association of the Study of Pain (IASP).
Furthermore, the results will inform further research proposals and planning, where we aim to undertake a controlled trial of virtual reality being used to manage chronic pain, with larger numbers of participants.
Potential of Virtual Reality for Chronic Pain
There is much potential for the use of virtual reality in helping individuals living with chronic pain, this is especially apparent when we consider the problems associated with long term use of opioids and the inability for pharmacological management alone to help these individuals.
It is clear that novel, affordable and accessible therapies are required to support individuals living with chronic pain.
Dr. Tarnia Taverner & Dr. Bernie Garrett
University of British Columbia
August 2015