Day one!
 (my view at lunch time everyday!)
(my view at lunch time everyday!)
I was more than nervous about taking the metro and walking to the school, but I was also excited. We all gathered in a lecture hall (after I got lost once or twice) and had an introduction lecture to the course leader and coordinators. Followed by the typical ice breaker exercises to meet a few people in the group. Today the schedule planned had three lectures. The first was General Introduction to Global health including disease patterns, second was Double burden of diseases followed by non-communicable diseases.
We received our books before class began as well and these are the ones they gave us (being from a non-medical student background.. oh boy.. I was a little intimidated)
Introduction:
Opening up the course we briefly touched on the millennium Development Goals. Listed under this title were:
- Eradicate extreme poverty and hunger
- Achieve universal primary education
- Improve maternal health
- Combat HIV/AIDS, malaria and other diseases
- Ensure environmental sustainability
- Reduce child mortality
- Develop a global partnership for development
Lecture one – Disease Patterns in developing and developed countries taught by Thor Theander.
Thor opened up by talking about the difference of disease prevalence and types of diseases (non-communicable and communicable) among developing and developed countries. We watched a short video presented by Hans Rosling on http://www.gapminder.org/ (this website is actually pretty interesting!) and here is the link for the video we watched http://www.gapminder.org/world/#$majorMode=chart$is;shi=t;ly=2003;lb=f;il=t;fs=11;al=30;stl=t;st=t;nsl=t;se=t$wst;tts=C$ts;sp=5.59290322580644;ti=1800$zpv;v=0$inc_x;mmid=XCOORDS;iid=phAwcNAVuyj1jiMAkmq1iMg;by=ind$inc_y;mmid=YCOORDS;iid=phAwcNAVuyj2tPLxKvvnNPA;by=ind$inc_s;uniValue=8.21;iid=phAwcNAVuyj0XOoBL_n5tAQ;by=ind$inc_c;uniValue=255;gid=CATID0;by=grp$map_x;scale=log;dataMin=194;dataMax=96846$map_y;scale=lin;dataMin=23;dataMax=86$map_s;sma=49;smi=2.65$cd;bd=0$inds=;example=60 (longer than I expected…) but it is really good at showing the changes that have occurred in life expectancy and how it is tied to income over the past 200 years. The really cool part is that you can change the axis.. so you can look at the changes in life expectancy to Infrastructure and “roads, paved (% of total roads) and see how that changes life expectancy over the past few years. It is quite fun to see how much has changed because such things as energy availability, infrastructure, cell phones and whatever else you can think of.
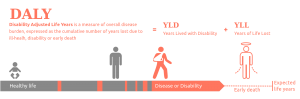
Thor talked about premature deaths – deaths occurring before the age of which the dying person would have lived to had then lived in Japan (Japan has the highest life expectancy at 90 years of age, so this is the golden measure of life expectancy for most comparisons). Healthy life lost due to disability is calculated by multiplying the number of years the person will live with the disability, by the percentage or weight of disability (this is pre-set and there is actually a chart giving a rating or ‘weight’ to all disabilities that qualify). An example of this would be a person with a lost finger would have a YLD (years living with disability) would be at 5% DW (disability weight) multiplied by the years they have not had their finger, but then someone who has lost their arm to accident would be at around 20% DW because this is more of a disability. Knowing the YDL is useful to calculate a DALY (Disability-adjusted life year), which is thought of as a lost year of “healthy” life due to disability or disease. It helps to measure the gap between current health status and the ideal situation of a full life to 90 years of age free of disability and/or disease. To calculate the DALY, you use the YDL calculated and add it to a YLL (year(s) of life lost, which is due to premature death (death occurring before 90 years of age). So to recap.. DALY = YDL + YLL, where YDL = DW x (duration of disability up to death or remission) and YLL = 90 – the age at death.
We touched on death causes and the percent/prevalence associated in developed and developing countries. There are noticeable differences seen. Tell me what you see!
| Developed Countries | Developing countries | ||
| Disease | % | Disease | % |
| Cerebrovascular disease and ischaemic heart disease | 37.8 | Cerebrovascular disease and ischaemic heart disease | 16.5 |
| Cancer | 9.5 | Lower respiratory infections | 9.9 |
| Chronic obstructive lung disease | 6.5 | Diarrhoeal disease | 7.4 |
| Traffic and suicide | 4.2 | Perinatal diseases | 5.1 |
| Diabetes | 2.4 | Tuberculosis | 5.7 |
| Malaria and measles | 3.9 | ||
| Chronic obstructive lung diseases | 2.7 |
When I look at the chart above I immediately notice one thing.. the difference between non-communicable diseases (NCD) and communicable diseases. As you may notice I highlighted the communicable disease in red there below the developing countries, but there are none highlighted, or even written in the developed countries column, why? Do you ever really hear about the disease and infections listed in large numbers? There was one outbreak of Measles in the Fraser Valley, BC – but other than that, really think about it.. Do you ever hear of people dying from these diseases listed in Canada or the US? No, you really don’t hear about them, maybe a few cases in a close knit area that spread quickly but then contained fairly quickly. Most of the time this is because so many people now are against vaccinations or feel that they are not necessary, not because they don’t have the option or can’t make it to a hospital to receive one like the children in developing countries.
We then went into difficulties of providing help for developing areas – to list a few: difficulty to reach certain areas, infrastructure is not there or damaged. Living conditions below the poverty level and economical resources are not enough or supplied. Education for providing the proper health care needed is not there and not available. Poverty and not having enough money to afford health care or medicine. Catastrophes, natural disasters and war in an area.
We compared the amount of money Tanzania has for the whole country in terms of health care and the amount of money Roskilde hospital (a small hospital located in Denmark) has. Can you guess the difference there is between a whole country and one small hospital? Well I was slightly shocked but Tanzania had and used $0.8 billion over the past year for the whole country, mostly coming from donors, charity and about 1/3 of this came from out of pocket expenses from the locals. Roskilde hospital had and used $0.6 billion over the past year. Does that shock you too? There are approximately 41 hospitals located in Tanzania (not including local health doctors, herb doctors and village doctors) that shared that budget of $0.6 billion, where as you can see and probably guess Roskilde is one hospital that stands alone with that budget.
Lecture 2 – Double Burden of Disease and NCDs in a Global Context by Ib Bygbjerg
Ib started out by introducing few key points, described by Omran in 1971. These points included how health and disease patterns change over time in societies, depending, among other factors, on the degree of:
- Demographic transition
- Rate of economic development
- Epidemiological transition
- Distribution of society
- Young society – infectious diseases and nutritional deficiencies dominate
- Children – diarrhea and acute respiratory infections (measles and malaria)
- Pregnant women – fetal loss, perinatal death from undernutrition, bleeding and infection
- Adults – TB and poverty related diseases
- Growing society (“growing up”) – accidence and violence-related disabilityes and deaths increase
- Infectious diseases and TB still prevail in young
- NCDs become more prevalent as urbanization increases and continues
- Aging societies
- NCDs predominate
- Type 2 diabetes and cardiovascular disease
- Cancer and degenerative disorders
- NCDs predominate
- Young society – infectious diseases and nutritional deficiencies dominate
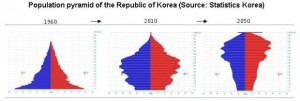
The above graph, represents the population of korea. In 1960 the population was heavily skewed towards children and youth (the skirt at the bottom), then in 2010 you see there is a buldge in the middle and then in 2050 a buldge at the top. What do you think this means? Well think about it this way, the young population has to age, and because of the high number of children and youth and high fertility rates at that time, people stopped having so many babies and the fertility rate went down. So the young population aged and that is seen in the buldge in 2010. Then again they aged and in 2015 the majority of the population will be elderly, that is.. if the fertility rate stays low. This is also a problem in many places like Japan and Iran for example. Both countries have implemented ways to increase fertility and increase their population again with younger children before their prevailing elderly populations die off.
Ib described and defined double burden. Before I tell you, what do you think he means with the saying “Double Burden of Diseases”?
- Ib said “it can be used to describe the emerging burden of NCDs and the non-decreasing amount of communicable (infectious) diseases, maternal and neonatal deaths and malnutrition”
An important slide we looked at and talked through for quite a while was this slide:
Disability-adjusted life years (DALYs) for 291 disease and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010 (Murray c. et al. Lancert2012;380:2197)
- Global disease burden has continued to shift away from communicable to non-communicable diseases and from premature death to years lived with disability
- In sub-Saharan Africa, many communicable, maternal, neonatal and nutritional disorders remain the dominant causes of disease burden
- The rising burden from mental and behavioural disorders, musculoskeletal disorders, and diabetes will impose new challenges in health systems
- Regional heterogeneity highlights the importance of understanding local burden of disease and setting goals and targets for the post 2015 agenda taking such patterns into account
At first glance – it is a lot of writing, but if you read it, it is showing that with urbanization is leading to the shift away from communicable to NCDs, with increases in mental and behavioural disorders as well as an increases in years lived with a disability but higher life expectancy (moving away from pre-mature deaths). In many areas urbanization is not happening, or it is not happening very fast so you still have high prevalence of communicable diseases. This can be a good thing, but it can also be a bad thing. The double burden is increasing as these two (NCDs and CDs) cross paths, causing many problems.
- Question asked by Ib: one un-prioritized, non-communicable disease plus one prioritized communicable disease in poor developing country in the tropics, which could benefit from integrated management and control, because of joint risk factors and interactions, which?
- Answer: TB and Diabetes
- Urbanizations increases risk for both, alcohol and smoking increase risk for both, TB increases risk of diabetes mellitus (DM) X2 and DM increase risk of TB X3
- BUT…. ‘DOTS’ = principles for TB management also works for DM
- A study done by Jeon CV & Murray MB (Plos Med 2008 – a systematic review of 13 observational studies) was a systematic review and meta-analysis of total of 1,786,212 participants with 17,698 TB cases showed:
- DM was associated with increased risk of TB
- The vast majority of TB patients (95%) and DM patients (70%) live in developing countries and this poses an extra challenge in terms of finding cost effective solutions
- The main challenge ahead for the double burder of TB and DM is to strengthen health systems – “primary health care in order to reduce the barriers for people with both disease to access quality health care” said Dr. Knut Lonnroth.
- Answer: TB and Diabetes
Another example we looked at was the balance of genetic polymorphisms (I had no idea what that meant when I first read it either, but then I remembered my BIOL 200 I took in college and clued in.. duh)
- Hb AS (hemoglobin – sickle cell trait) à protection against severe malaria
- Hb SS (sickle-cell disease)à increase susceptibility to malaria, haemolytic crises, aplastic crises, splenic infarctions, functional asplenism à death
- Thalassaemia (form of inherited autosomal recessive blood disorder – abnormal formation of hemoglobin), minor à protection malaria
- Thalassaemia, major à haemolytic anaemia, hydrops foetalis, death before birth or early neonatal life
- Glucose-6-phosphate dehydrogenase deficiency G6PD à protection against severe malaria, but may increase risk of diabetes
Examples of infections and NCD’s
- Parasites and cancer
- Schistosomiasis à urinary bladder cancer
- Chlonorchiais à gall-duct cancer
- Parasites and autoimmune diseases
- Malariae à nephrotic syndrome
- cruzi à Autonomous nerve destruction
- Mega-syndrom : cardiomegaly, mega-oesophagus, mega-colon à arrhythmia cordis, heart-block à sudden death
- Parasites and anaemia
- Virus and immunosuppression
- Infections in utero and diabetes/hypertension
- Bacteria and ulcus disease (peptic ulcer)
To finish the day we discussed “Word of warning” – what? Warning for what?
- A double burden of disease requires integrated balanced control strategies that should begin in the primary health care sector
- Integration requires maximum involvement of all specialized personnel
Suggestions:
- Look for joint risk factors AND joint management tools
- Adapt – control and management to the primary health care system
- Adopt – link an orphan or neglected disease with other diseases, when obvious joint manifestations or complications, by integration control and management
There is a need globally and locally for a life-cycle approach to prevent and manage infections, injuries and NCDs. The life-cycle looks like this
- Fetal health (affected by nutritional and/or infections) linked into
- Child health (affected by infection) linked into
- Adolescent’s health (affected by injuries and accidents) linked into
- Adult/father/mother’s health (affected by NCDs and mental health) linked into
- Elderly health (affected by NCDs) linked back to fetal health à making this a cycle
And finally! The conclusion:
- Genes and ethnicity may impact susceptibility to infectious disease as well as to NCDs
- Other risk factors and determinants including socio-economic determinants are more often of importance
- Rapid changes in living condition and life-style including factors next to the genes, namely epiges may adopt to these changes, whereas genes only change very slowly by mutations of by selection pressure
- Maladaption to new environments are probably major drivers of changing patterns of disease
 This is Brendan and myself. Brendan is a doctor from Holland and a very interesting person to hang out with and go exploring.
This is Brendan and myself. Brendan is a doctor from Holland and a very interesting person to hang out with and go exploring.
 The view along the inner city canals.
The view along the inner city canals.
 The outer city limit of the area of Copenhagen that I live in currently with my 3 other roommates. They are all doctors, so I am learning quite a bit from them while I am here as well 🙂
The outer city limit of the area of Copenhagen that I live in currently with my 3 other roommates. They are all doctors, so I am learning quite a bit from them while I am here as well 🙂