Having any experience in the biomedical sciences, the phrase “microscopy is a lost art” must have some meaning to you. It means biotechnology is taking over the medical sciences. Biochemistry and molecular biology have become so prominent that techniques of old are being replaced by all things molecular.
Recent advancements in biotechnology have revolutionized science. DNA experiments not only conduct replication, they incorporate automatic interpretation of the results. Protein science has been simplified to pouring samples in vials and running them in a machine, no further skills or education required. Even medical diagnostics are “going molecular”, using DNA and protein experiments to diagnose patients rather than the traditional interpretation of labs. But while molecular experiments sure make our lives (as a scientist) easier, haven’t we been taught that shortcuts are never the answer?
What’s wrong with going molecular?
A perfect example to illustrate this point is with the blood infection: malaria. Annually, an estimated 600 million people globally still suffer from this parasitic disease and over a million die from it. Current diagnostic methods involve blood smears under microscopy as shown in the photo below; the purple specks representing malaria parasites.
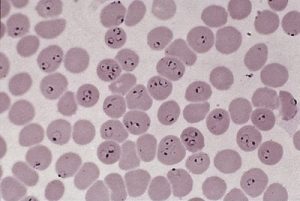
Picture by Teresa Lo, BCCDC
However, when presented to pathology residents of UBC’s Faculty of Medicine, not a single one of them could identify the illness. Even more astonishing, they actually thought that the patient was perfectly healthy. This incident occurred at the BC Centre for Disease Control, where technicians of the Parasitology department tested medical residents with confirmed-diagnosis patient samples.
How did this happen?
With advancements in science and technology, biotech companies have developed molecular tests for diagnosing patients. For malaria, a well-known device is called the Rapid Test shown below. Functioning like a pregnancy test with urine, the Rapid Test simply requires a drop of blood and some time before a positive or negative result is given. You might be asking “where’s the problem?”. While the Rapid Test IS very convenient, it has a relatively low success rate. This is further discussed on the CDC website for malaria diagnosis.

Picture by Benjamin Chang, BCCDC
For patients where the malaria parasite is not prevalent or perhaps has not replicated enough, detection via Rapid Tests would fail. This is why microscopy is so important in the field of parasitology, it can detect parasitemia at low enough concentrations that early intervention would be possible. A paper published in the Journal of Malaria found microscopy was a better method for diagnosis compared to molecular techniques:
Biomedical scientist Emmanuel Biney further demonstrates in this video that while the skill required for microscopy is high, it is most definitely required:

Unfortunately, microscopy is truly a lost art as our generation is geared towards molecular techniques. Training in microscopy takes numerous years of practice and an experienced technician as an instructor. As the previous generation retires and our generation begins to enter the workforce, we will have to find some way to compensate for the loss of their skills.
