HIV and its Implications
The HIV global pandemic was once a major killer in the 20th century. HIV causes mental panic, social apprehension mortality when left untreated and miseducated. Due to the fact that diseases transmitted from sexual contact or drug usage cause social stigma, the HIV global pandemic became a fight not only against the virus itself but the perception of that from the general public. Though no form of illness should be conceptualized from that of a negative connotation, HIV long has had a conception coming from promiscuity, drug addiction, and carelessness. Treatment for HIV and better education continues to be a global battle.
HIV is described as a virus with no cure but treatable. Proper treatment of HIV can allow an infected individual to live a normal lifespan. Source: HIV.gov
How HIV is Transmitted
HIV is transmitted through sexual contact, needle sharing, contaminated blood transfusion as well as birth. HIV is a virus that attacks the body’s immune system. The latent stage of HIV is AIDS when the CD4 cell count in the body lowers to rates that cause infections to be prone.

HIV is transmitted through four major ways: sex, blood transfusion, needle sharing and mother to baby. Source: avert.org
Treatment History
HIV treatment first began with Zidovudine, which became available in 1987. Zidovudine causes side effects such as low blood cell count, liver damage. More importantly, Zidovudine stops working as the virus mutates. In 1996, antiretrovirals became available for public use. The combination of antiretrovirals made it difficult for enzymes in HIV to replicate. In 2007, Raltegravir became available as an HIV integrase inhibitor. In 2010, Truvada became an available option for pre-exposure prophylaxis for the public.
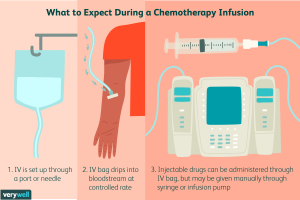
New Injection Treatment
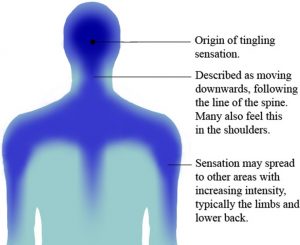
Treatment for those infected with HIV requires a daily oral pill. Until 2021, one of the oral pills had to be taken by someone HIV positive. A daily pill makes it difficult to adhere to treatment. Moreover, oral pills are difficult for those with swallowing difficulties, poor drug absorption, and gastrointestinal problems. Cabotegravir and rilpivirine are taken as integrase inhibitors and non-nucleoside reverse transcriptase inhibitors. These two medications are taken in injection form once every one or two months. The result is that injection forms require much less dedication to HIV treatment, as these forms don’t require a daily treatment plan. The key to HIV treatment to allow those living with the virus to lower transmission and keep the virus under control is to have an undetectable viral load. An undetectable viral load allows an infected person to live a normal lifespan and be HIV non-transmissible. Injection treatment works equally as well as the oral pill.

HIV injection Treatment Description
New Treatment Plan
In the UK, injection treatment for HIV will begin in 2022. Other European countries are soon to follow this plan. Another treatment plan for HIV is a solution and alternative to approach a virus in modern society.