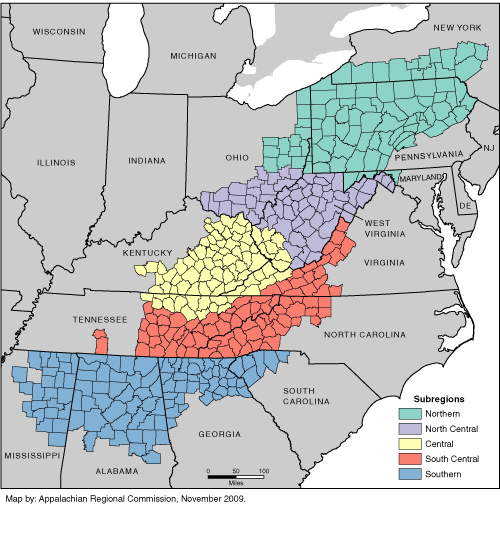
Lung cancer is the second most commonly diagnosed form of cancer in the United States (Centers for Disease Control – CDC, 2018). It is the leading cancer killer in both men and women, accounting for approximately 27 percent of all cancer deaths (American Cancer Society, 2018; Siegel, Miller, & Jemal, 2016). It also has the greatest geographic variation of all cancers across the United States (Siegel et al., 2016). Incidence and mortality rates vary widely; however, counties in the southeastern states generally have higher rates of smoking and lung cancer mortality (CDC, 2002; Lengerich et al., 2005; Wingo et al., 2008). Many of these counties are part of the Southern and Central Appalachia, geographic sub-regions noted for high poverty rates, limited access to healthcare, low education attainment and coal-mining (Halverson & Bischak, 2008) (Figure 1.1). It is important to recognize, as several recent studies have pointed out, that smoking alone cannot explain the high rates of cancer mortality observed at the regional or national scale (Christian, Huang, Rinehart & Hopenhayn, 2011; Hamra et al., 2014; Sun, Schiller, & Gazdar, 2007).
Figure 1.1
The scientific consensus clearly dictates that smoking is the leading cause of lung cancer across the United States. It contributes to 80 percent and 90 percent of lung cancer deaths in women and men, respectively (Office of the Surgeon General, 2004). Exposure to secondhand smoke at home or work increases the likelihood of developing lung cancer in non-smokers by 20 to 30 percent (CDC, 2014). This contribution to lung cancer rates is particularly evident in the Midwest and South, where smoking prevalence is higher and a greater percentage of smokers smoke more than a pack a day, relative to the rest of the country (Christian et al., 2011; Jamal et al., 2018; Orzechowski & Walker, 2014). Aside from smoking, other environmental exposures and socioeconomic factors may be associated with observed patterns of lung cancer incidence and mortality. For instance, exposure to air pollution has been linked to a variety of lung diseases, including cancer (Turner et al., 2011). Radiation also contributes to lung cancer incidence. According to the Environmental Protection Agency (EPA), radon is the primary cause of lung cancer in nonsmokers and the second leading cause of lung cancer overall (EPA, 2018). Much of the United States is classified as a high risk radon zone, where indoor radon levels are expected to exceed the target level of 0.4 picocuries per litre (EPA, 2017). Incidence of lung cancer also varies within demographic and socioeconomic categories of wealth, race, education, and gender. For example, black men and women are more likely to develop and die from lung cancer than persons of any other racial or ethnic group. Interestingly, the age-adjusted lung cancer incidence rate among black men is approximately 28 percent higher than for white men, despite a lower overall exposure to cigarette smoke (the primary risk factor for lung cancer) (Chatila, Wynkoop, Vance, & Criner, 2004; Howlader et al., 2016). The cancer incidence rate for black women is roughly equal to that of white women despite smoking fewer cigarettes (Chatila, et al., 2004; Howlader et al., 2016). Differences also exist along gender lines; men are significantly more likely to be diagnosed with lung cancer than women (Howlader et al., 2016). Increased risk of lung cancer incidence has also been observed among people with low educational and/or low income-based socioeconomic positions (Sidorchuk et al., 2009).
This study was conducted in order to answer the research question: How are lung cancer mortality rates associated with environmental and socioeconomic factors across the eastern United States? Our analysis focuses at the turn of the century (1999), when long-term trends of American male and female lung cancer mortality rates had reached peak levels and begun to decline (Siegel et al., 2018). Eastern states were chosen because of their higher rates of mortality, particularly in the Appalachian region. The distribution of relevant environmental and socioeconomic factors, and their corresponding association with lung cancer mortality, varies widely across space. Therefore, the analysis was conducted at the county level in order to reveal local-scale patterns.