7 Customers Showed Symptoms of Scombroid Fish Poisoning after Eating in a Sydney Café
Seven people fell ill and showed symptoms of scombroid poisoning after eating from the same food outlet in the Sydney CBD, Soul Origin café, in late February 2015. The tuna, which was served in sandwiches at the café, was suspected to have caused scombroid poisoning.
source: http://www.abc.net.au/news/2015-02-26/scombroid-fish-poisoning-linked-to-sydney-cafe-tuna/6263120
The New South Wales (NSW) Food Authority in Australia investigated that the canned product “John Bull Tuna Chunky Style in Sunflower Oil”, which Soul Origin café used, is a product of Thailand and imported into Australia by a Victorian company. This minor brand was used predominately in catering; it was not generally available to the public. The outbreak was not widespread and all affected product was removed from the market immediately.
source: http://ausfoodnews.com.au/2015/03/11/canned-tuna-food-safety-scare-linked-to-thai-factory.html
The NSW Food Authority tested the leftover tuna salad at the café to have 3950 micrograms of histamine per kilogram of tuna. The test result was well above the acceptable limit of 200 micrograms histamine per kilogram of fish.
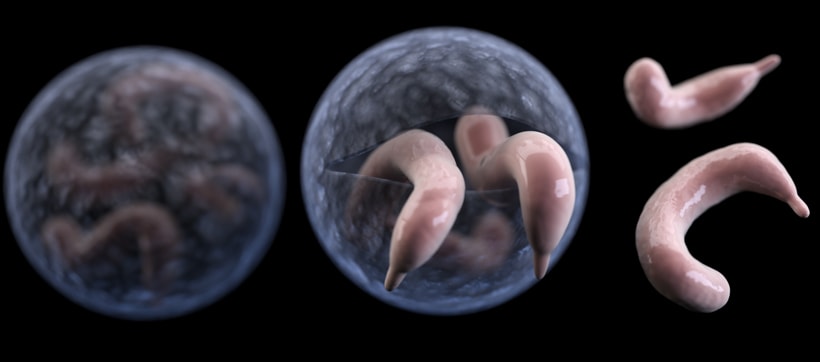
Scombroid poisoning is an allergic-type reaction to elevated levels of histamine in fish. It occurs when an enzyme produced by naturally occurring bacteria in certain fish species (including tuna, sardines, mackerel, swordfish, and marlin) convert histidine in the fish to histamine. Elevated levels of histamine amino acids in the fish produce cause the food poisoning. The temperature abuse of the fish produce at the catching or processing stage is usually the cause of the scombroid poisoning. The presence of high level of histamine in fish shows that decomposition of fish produce has occurred. The histamine toxin is not inactivated by ordinary cooking methods, and the contaminated fish will not necessarily appear spoiled.
Symptoms of histamine poisoning occur quickly, usually within 30 minutes or a few hours upon ingestion of contaminated fish. The symptoms typically last for a few hours. However, in some cases, they can last for several days. Common symptoms of histamine poisoning including peppery or metallic taste sensation, tingling of mouth and lips, skin rash or itchy skin, headaches, and dizziness; nausea, vomiting and diarrhea may also occur in some cases. People with scombroid poisoning may be treated with antihistamines. Scombroid poisoning is rarely fatal, but it was thought to have killed a Australian mother and daughter, Noelene and Yvana Bischoff, while they were on vacation in Bali in January 2014. However, the case is extremely rare.
Here is the news article on the tragedy happened in Bali:
http://www.news.com.au/national/bali-deaths-of-noelene-and-yvana-bischoff-from-fish-poisoning-impossible-to-predict/story-e6frfkp9-1226818860731
Histamine poisoning is rare, and there have been less than 10 outbreaks of histamine poisoning with 187 people diagnosed with the poisoning in Australia over the past 10 years.
Since histamine is not destroyed by heat treatments, buying seafood from reputable sources to ensure the product is kept refrigerated when it is being transported and stored becomes the best way to protect us against scombroid poisoning.
News sources & Reference:
Australian Broadcasting Corporation, 2015. Scombroid Fish Poisoning Linked to Sydney Café after Four Customers Fall Ill. Retrieved from http://www.abc.net.au/news/2015-02-26/scombroid-fish-poisoning-linked-to-sydney-cafe-tuna/6263120
Australian Food News, 2015. Canned Tuna Food Safety Scare Linked to Thai Factory. Retrieved from http://ausfoodnews.com.au/2015/03/11/canned-tuna-food-safety-scare-linked-to-thai-factory.html
Canadian Food Inspection Agency, 2012. Food Safety Facts on Scombroid Poisoning. Retrieved from http://www.inspection.gc.ca/food/information-for-consumers/fact-sheets/food-poisoning/scombroid/eng/1332280657698/1332280735024
Daily Mail Online, 2014. Australian Mother and Daughter Who Died in Bali Hotel Room Victims of Rare Fish Poison. Retrieved from http://www.dailymail.co.uk/news/article-2551853/Australian-mother-daughter-died-Bali-hotel-room-victims-RARE-fish-poison-combined-asthma.html
Food Standards Australia New Zealand, 2015. Histamine (Scombroid) Fish Poisoning. Retrieved from http://www.foodstandards.gov.au/consumer/safety/Pages/Histamine-(Scombroid)-fish-poisoning.aspx
New South Wales Food Authority, 2015. Update: NSW Food Authority Investigation into Scombroid at Sydney Café. Retrieved from http://www.foodauthority.nsw.gov.au/news/media-releases/mr-26-Feb-15-scobroid-sydney-cafe#.Vk_Ii0ujZ4U










 Cholera, an infection that is commonly found in central Africa, has affected thousands of millions of people every year, according to the World Health Organization (WHO). Cholera is an acute diarrheal disease that is caused by the strains of a bacterium called Vibrio cholerae. V. cholerae is a pathogen that colonizes the small intestine and causes symptoms such as watery diarrhea and vomiting. If left untreated, people will suffer from severe dehydration and leads to death within hours.
Cholera, an infection that is commonly found in central Africa, has affected thousands of millions of people every year, according to the World Health Organization (WHO). Cholera is an acute diarrheal disease that is caused by the strains of a bacterium called Vibrio cholerae. V. cholerae is a pathogen that colonizes the small intestine and causes symptoms such as watery diarrhea and vomiting. If left untreated, people will suffer from severe dehydration and leads to death within hours.
 The method people use to treat cholera is by oral rehydration salts (ORS), a treatment that is indicated by WHO. Severe diarrhea will leads to dehydration so ORS is a very effective and efficient way on rehydrating people. Anitibiotics are also used to shorten diarrhea duration. To control the outbreak of cholera due to weather such as raining season, they will introduce cholera vaccines to people. The following video shows the situations people are facing in Africa and how they are treating cholera using vaccination. In order to prevent cholera outbreak, improving sanitation and access of safe drinking water are the keys, which are also indicated on the video. We shall not neglect the importance of improving environmental conditions such as household hygiene, water filtration, development of water pipe system by treating disinfectants, etc. These strategies can upgrade their living conditions and minimize the chance of getting infected.
The method people use to treat cholera is by oral rehydration salts (ORS), a treatment that is indicated by WHO. Severe diarrhea will leads to dehydration so ORS is a very effective and efficient way on rehydrating people. Anitibiotics are also used to shorten diarrhea duration. To control the outbreak of cholera due to weather such as raining season, they will introduce cholera vaccines to people. The following video shows the situations people are facing in Africa and how they are treating cholera using vaccination. In order to prevent cholera outbreak, improving sanitation and access of safe drinking water are the keys, which are also indicated on the video. We shall not neglect the importance of improving environmental conditions such as household hygiene, water filtration, development of water pipe system by treating disinfectants, etc. These strategies can upgrade their living conditions and minimize the chance of getting infected.

ColleenChong 8:14 pm on November 22, 2015 Permalink |
Very interesting article! I really like how you were display two cases of Scombroid fish poisoning to display the common reason that this food-borne illness occurs. From the two articles storage and transportation temperatures of fish seems to be crucial since it is due to bacteria converting histidine to histamine. As you have mentioned that the production of histamine is often due to the decomposition of the fish. I think that it is important that Health authorities do increase monitoring of quality of imported fish and histamine levels. Although the cases of scombroid poisoning seems to be rare it might occur without detection because the symptoms of poisoning is common with other illnesses. I think increasing the surveillance of Scombroid fish poisoning would be beneficial to the public because it is a preventable food-borne illness through proper manufacture, retail and consumer practices.
Susanna Ko 12:27 am on November 24, 2015 Permalink |
That is really unfortunate because the high levels of histamine are not reduced with cooking, so it’s really about the handling of the raw fish prior to processing it. I thought that the food processing plant would test their raw and finished products on the histamine levels. One would think that regulations and HACCP would prevent this kind of occurrence, especially in ready-to-eat hermetically sealed canned foods.
amreenj 3:19 pm on November 30, 2015 Permalink |
Great article! It is scary to see how much histamine there really was in the left over tuna, having 3950 micrograms/ kg is well over the acceptable limit of 200 micrograms/kg and could lead to severe complications as a result. Often with temperature abuse, it may be difficult to tell that this has occurred unless there are distinct/ obvious signs such as spoilage, odour, or colour change. I would think that there would be measures in place to firstly prevent this from happening, secondly to prevent this type of fish from being packaged, and thirdly that once opened chefs are able to detect that there may be something wrong with a fish (ie. if there is odour etc.). Histamine reactions can be fatal and as such, extra precautionary measures must be in place to prevent such things from occurring.
Mandy Tam 9:35 pm on December 1, 2015 Permalink |
This article provides a lot of good information about seafood poisoning. I have learn a lot.
I know CFIA tracks histamine level in all imported fish products from the tour I have in FNH 326 in CFIA. CFIA has a specific import inspection program and one must get a fish import license to permit to import and sell fish in Canada. If someone is selling fish to restaurant or retail store without permit, he/she might be on conviction by indictment. The person might need to face jail time or/and paying a fine. Therefore, there is extensive tracking in Canada. I wonder what is the regulation/ surveillance Australia has on preventing fish poisoning from imported food. Anyhow, this is a very lucky case that no one died because of the outbreak.
Link to CFIA:
http://www.inspection.gc.ca/food/fish-and-seafood/imports/eng/1299825431569/1299825501933
elaine chan 12:08 am on December 2, 2015 Permalink |
Interesting article! I liked how you provided a detailed explanation as to what scombroid poisoning is, and its relation to histamine levels. I find it really amazing how a product containing 3950mg of histamine per kg of tuna was even allowed to be distributed for sale, when it’s way over its acceptable limits. It makes me question whether the manufacturer of this product performs quality control testing to ensure that their product is safe for consumption. Thankfully, this product was not for sale that’s available to the general public, or else its consequences would have been much, much more severe. However, it still caused a food borne outbreak that I felt could’ve been prevented through more strict quality control measures. I hope that the cafe does not suffer a major customer loss from this incident because they are the innocent victims. They are the consumers, and typically in cafes or restaurants, products such as canned tuna, are purchased with the assumption that they are safe and ready for consumption. I feel that both Thailand and Australia should implement more strict surveillance to ensure that exported and imported food products are safe for the general population for consumption.
flyingsquirrel 4:35 pm on December 2, 2015 Permalink |
What I find interesting about this article is that it shows that it is not just bacterial pathogens that produce toxins that are harmful once consumed (for example Clostridium botulinum, dinoflagelettes ). There are many naturally occurring endogenous substances that are potentially toxic in high amounts and I am glad this article brings that into light. I think many people in general that do not work or study in food safety will often overlook this and it is important to be aware that proper storage of foods is not only important for preventing bacteria proliferation, but also for preventing unwanted enzyme activity to keep foods delicious and safe. I think one reason why the monitoring of the tuna products imported seems inefficient may be due to the fact that it is not sold in the mass public market. Perhaps allocated resources left for inspecting certain products were unequally distributed based on the size of the target market?
YaoWang 12:17 am on December 15, 2015 Permalink |
It’s interesting that people can get sick by eating “allergic” fish. But it’s unfortunate to know that we can neither get rid of the histamine through normal cooking methods nor distinguish between fresh and spoiled fish. Apparently the problem can be caused by many microorganisms, rather than just the pathogens and therefore, is of great concern. So, I’m wondering what we could do to prevent such food-borne illnesses in the future?
CandiceZheng 2:37 pm on December 15, 2015 Permalink |
Thank you for sharing the seafood poisoning case with us! And I personally feel it is very unfortunate that although we understand that histamine level can indicate the degree of seafood decomposition, for the normal population there is no easy way to differentiate whether there is high level of histamine on the seafood. As indicated in the post, the leftover tuna salad at the café have 3950 micrograms of histamine per kilogram of tuna, which is well above the acceptable limit of 200 micrograms histamine per kilogram of fish. However, people still couldn’t observe any unusual appearance from these tuna. In this case I think it is very important to have some quick and easy way to examine the histamine level on seafood. For example, using something like pH test strips that are cheap, easy to use, and handy for the general population to use to test the histamine level on seafood in order to prevent further poisoning issues.
DeniseZhang 7:37 pm on December 15, 2015 Permalink |
According to the food chemistry courses that I am taking this term, histamine is a product from decarboxylation reaction of histidine. On immunological aspect, histamine can cause inflammation in human bodies (which is good while fighting pathogens), and it can also lead to hypersensitivities (a.k.a. allergy) in human bodies. I did not know that we have histamine poisoning issue in our life. Even though it is an extremely rare case, I do believe that we need to pay attention to it as undesirable inflammation is annoying. I really wish food provides can know more about those potential risks in foods, so that we can have foods more safely.