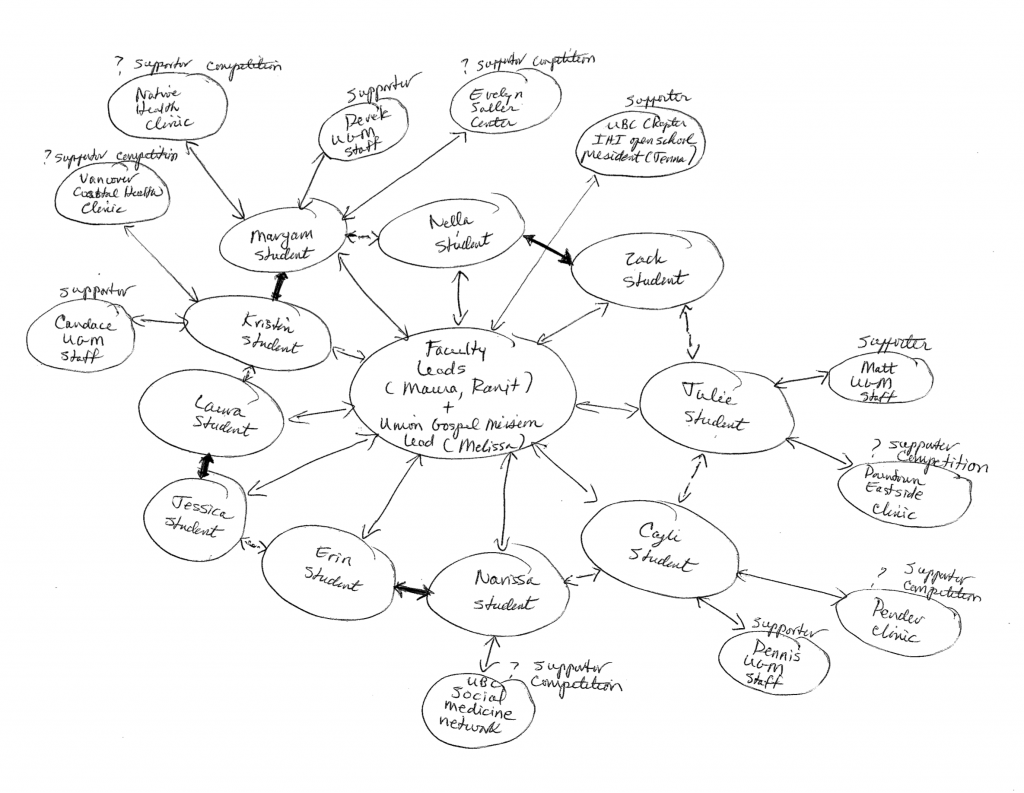
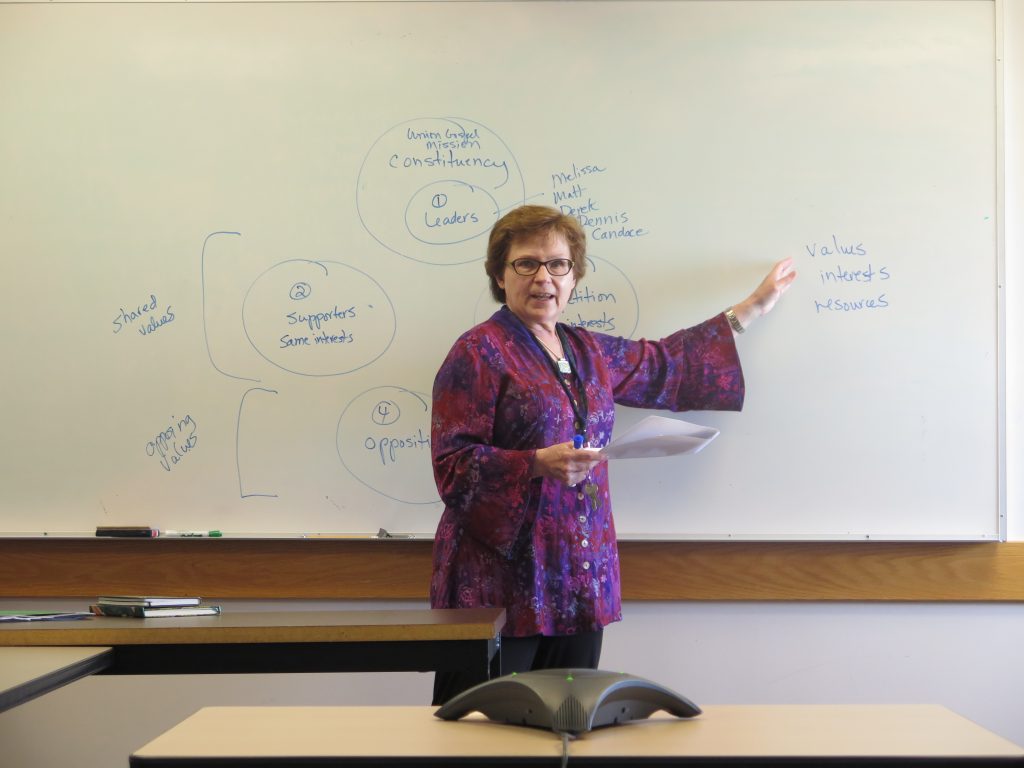
The I-CAN project started as collaboration between two UBC School of Nursing faculty members, Maura and Ranjit, and the Director of the Union Gospel Mission (UGM), Melissa.
Maura and Ranjit posted a notice about the I-CAN project, and 10 students signed up for the project. The 10 students are those circles closest to the center of the snowflake.
In an initial project meeting between Maura, Ranjit and Melissa, Melissa identified the need for a sustainable foot care clinic. The School of Nursing currently does foot soak clinics every 6 weeks. This activity is very popular at UGM, but the staff and clients would like to expand available services, based on client requests for professional foot care.
Melissa suggested that we begin our project by talking with UGM staff and getting them on board. Four student volunteers interviewed these UGM staff. UGM staff members provided additional names of inner city clinics that might partner with us on this project. The students are setting up interviews with these clinics to determine whether or not they are supporters or competitors. These inner city services are in the next layer of the snowflake with ?s (competitor, supporter). We hope to win them over to our project!
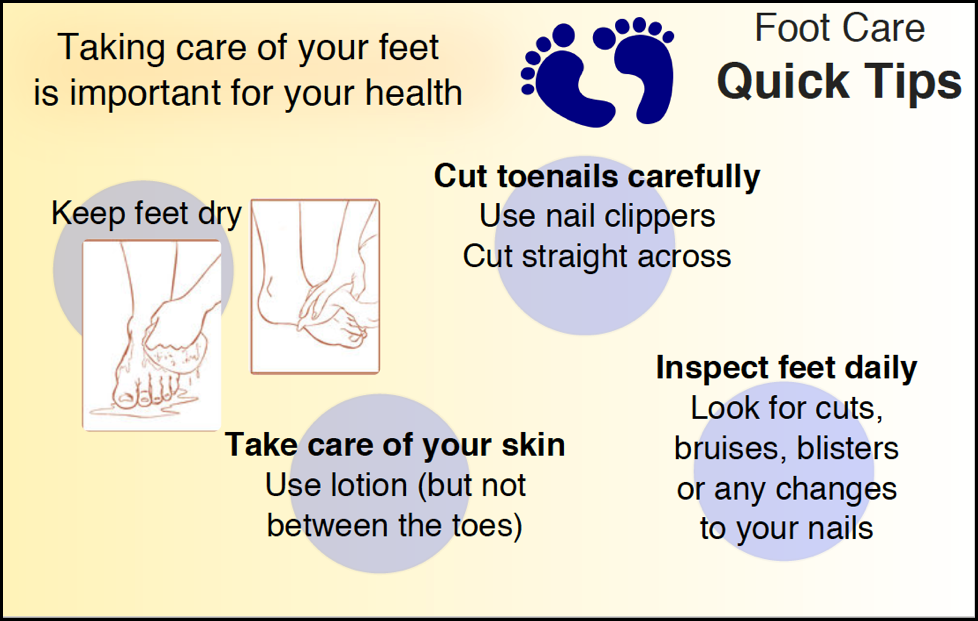
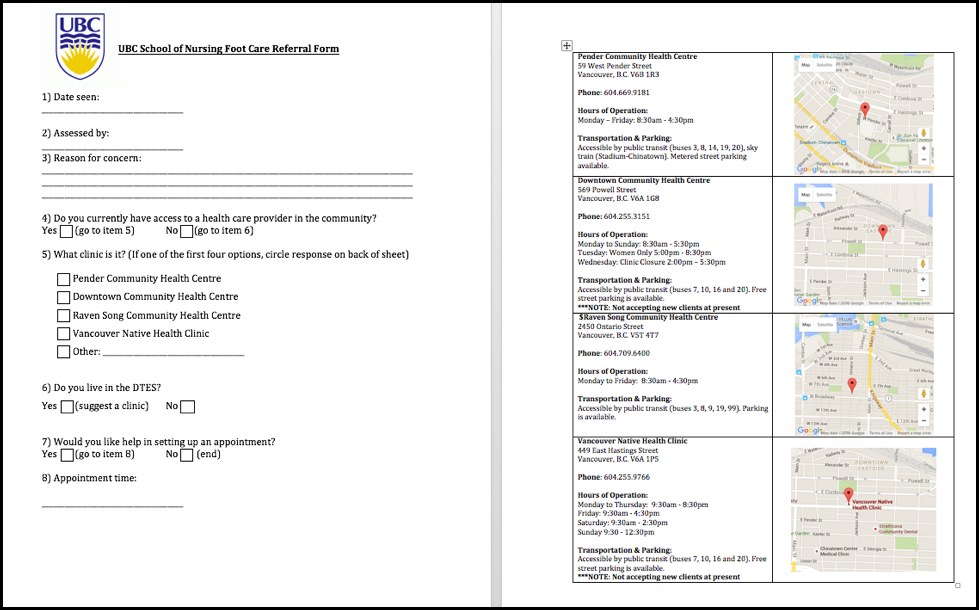
Our asks are: 1) Are there professionals who can do foot assessments? 2) If so, would they be willing to volunteer their services every 6 weeks during the School of Nursing foot soak clinic? 3) Would they be willing to review the accuracy, utility of deliverables we create through this project? (We are creating a “Foot Care Tips” card and a referral form for UGM clients).
The bold lines between students indicate students who are working together on interviews or other aspects of the project. Melissa and UGM staff members have asked for a “Foot Care Tips” card to give to clients during foot soaks—a teachable moment for students doing client foot soaks. Two students are designing this card.
The UGM staff members have also asked us to create a standardized referral form to connect clients with foot disorders to inner city services. We need to identify inner city service providers who will receive UGM referrals, and we need to set up a standardized process for referrals to happen smoothly, efficiently. Two students are working on the referral form.
A third deliverable for this project will be a video of foot assessment: for all foot care clinic volunteers to watch. The UGM staff members (and UBC faculty) want to ensure that anyone volunteering for the clinic has basic information about foot assessments and specific issues for the UGM client population. Our intention is to ask service provider supporters to review and approve our three deliverables (i.e., foot care tips card for clients, referral form for inner city foot care services, and a video for foot care clinic volunteers).
The UBC faculty leads have been having conversations with the UBC chapter president of IHI Open School. They are discussing the possibility of making the foot care clinic an initiative of the UBC chapter. One student, a member of the UBC Social Medicine Network, is also talking with members of this student association to determine inter-professional student interest in our foot care clinic.
We realize that our snowflake will continue to grow as we establish more contacts and relationships with services (non-profits and for-profits) in our inner city area.
We have a question: We have not included the UGM clients as part of our team. We are, however, having regular discussions with them about the services they want, and we will ask for their input and feedback on our project deliverables. Should they be included in the snowflake?
 Follow
Follow

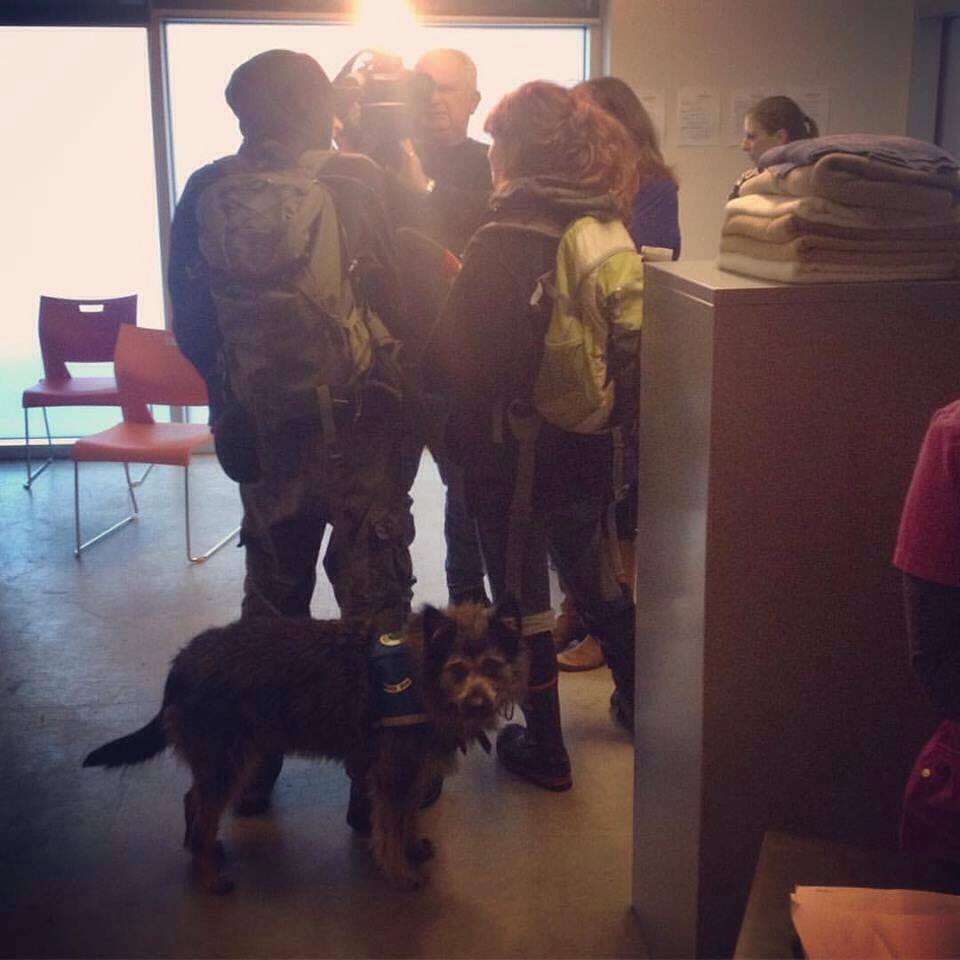



 Our foot soak service offered clients accessing the lunch service to soak, clean and have their feet massaged and dried thoroughly, and to get a new pair of socks; a small action that goes a really long way in Vancouver’s damp weather. During this time, the UBC student nurses were able to engage with clients, assess their foot health, talk about their general health and their concerns and make a referral to primary health care services in the community if desired and indicated. Simultaneously, students were able to get to know some of the real people living in this community and were able to gain some understanding of how social positions intersect as the social determinants of health can impact an individual, a community and populations health and well-being. Every six weeks students working through their community health rotations would cycle through and participate in hosting the foot soak clinics.
Our foot soak service offered clients accessing the lunch service to soak, clean and have their feet massaged and dried thoroughly, and to get a new pair of socks; a small action that goes a really long way in Vancouver’s damp weather. During this time, the UBC student nurses were able to engage with clients, assess their foot health, talk about their general health and their concerns and make a referral to primary health care services in the community if desired and indicated. Simultaneously, students were able to get to know some of the real people living in this community and were able to gain some understanding of how social positions intersect as the social determinants of health can impact an individual, a community and populations health and well-being. Every six weeks students working through their community health rotations would cycle through and participate in hosting the foot soak clinics.