“I had the pleasure of meeting Elder Don while UBC Nursing students were engaged in health promotion teaching at the Turing Point in Richmond. Elder Don and I quickly established a trusting friendship as he shared life stories. I invited Elder Don to the N336 classroom to share his lived experiences of being in residential school, foster homes and living in marginalized conditions in the Down Town East Side (DTES) Vancouver. Through his stories Elder Don encouraged students to become kind compassionate non judgmental health care practitioners. On behalf of the N336 class ( Rotation A 2017) and UBC SON we thank Elder Don for so willingly to share his life story to enhance student learning”. –Ranjit Dhari, N336 Course Leader 2017
“I had the pleasure of meeting Elder Don while UBC Nursing students were engaged in health promotion teaching at the Turing Point in Richmond. Elder Don and I quickly established a trusting friendship as he shared life stories. I invited Elder Don to the N336 classroom to share his lived experiences of being in residential school, foster homes and living in marginalized conditions in the Down Town East Side (DTES) Vancouver. Through his stories Elder Don encouraged students to become kind compassionate non judgmental health care practitioners. On behalf of the N336 class ( Rotation A 2017) and UBC SON we thank Elder Don for so willingly to share his life story to enhance student learning”. –Ranjit Dhari, N336 Course Leader 2017
by ERICA BENSON
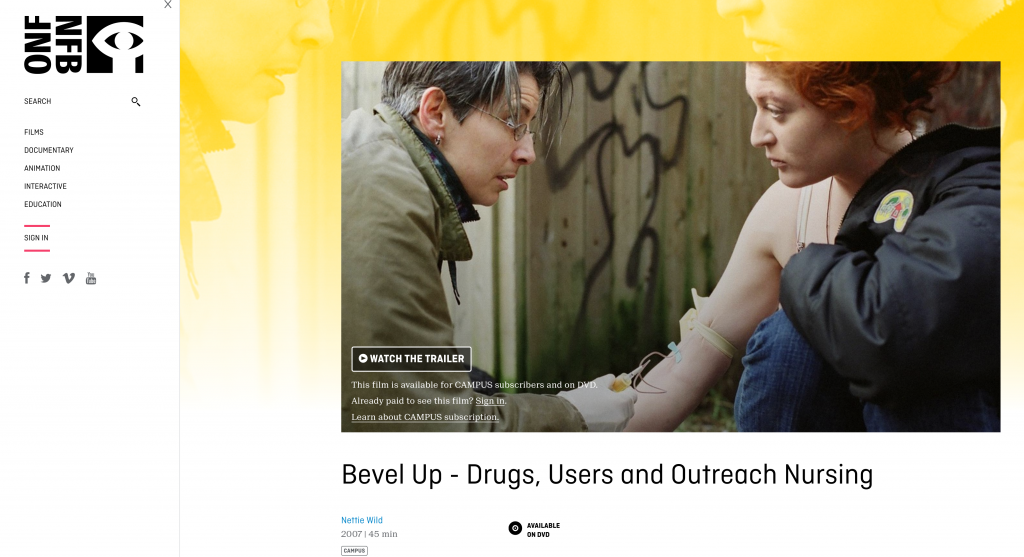
“Bevel up,” a street nurse says to a young man in an alley of Vancouver’s Downtown East Side (DTES) in a documentary by Nettie Wild. The nurse is pointing to the side of the needle he should insert in his arm when injecting drugs. The outreach nurses interact with residents of the DTES in an attempt to increase health care services and build trust with a population where many have been failed by our health care system. The documentary revealed there exists a population of people unjustly profiled, mislabeled, and mistreated by health care professionals here in British Columbia.
Without an understanding of the pathways to homelessness and addictions, the factors that contribute to the intergenerational trauma of First Nations communities and ongoing structural systems in place that keep the oppressed, oppressed; student nurses run the risk of perpetuating the mistreatment of marginalized populations. Elder Don, a Dene First Nations Elder, brought his amazing story of hardship and perseverance to illuminate the challenges he faced while experiencing addiction and living on the streets of the DTES.
“People don’t necessarily want to confront these issues…it forced students to hear something that is hard to hear,” said one student. “People talk about truth and reconciliation and they want the reconciliation but not the truth. It’s too hard.” they continued, baring a sensitive dichotomy that exists concerning First Nations issues in Canada.
Across Canada, depending on their upbringing and school curriculum, students may not even learn about residential schools. Kait Kilyk from Fonthill Ontario found the presentation illuminating and inspiring. “My knowledge of residential school prior to the presentation was quite limited. I was aware of some scenarios from previous documentaries but never had the opportunity to discuss with someone their experiences in the school.”
Elder Don was taken from his family and community, forced into residential school, and then placed into foster care. First Nations children in residential schools had their hair cut, were punished when they spoke their language, segregated from their siblings and too often were sexually, emotionally and physically abused. Today, First Nations children still suffer. A report in 2011 by Statistics Canada revealed that First Nations children make up 48% of children in foster care in Canada, grossly over representing any other group in care. In 2016, the Canadian Human Rights Tribunal ruled that the Canadian government is discriminating against First Nations children by providing flawed, discriminatory and inequitable health care services which is a violation of the Canadian Human Rights Act. To date, Prime Minister Trudeau announced a 5-step plan to implement the Tribunal and the Truth and Reconciliation Committee’s call to action, however progress is slow and in the meantime First Nations children bear the brunt of the inaction, many ending up homeless. Creating a safe space to answer our questions, Elder Don challenged our preconceptions about homelessness and offered insight to First Nations culture.
“Why did you sleep outside?” a student asked Elder Don during the presentation.
“Shelters are crowded, a big room full of beds, with bed bugs and scabies and you have no personal space. I preferred living outside under the stars, I didn’t mind it.” Elder Don replied, sharing some downfalls of the systems in place meant to be salvation for homeless individuals.
Seohee Lee, a global citizen from South Korea related to Elder Don in her desire to work coming from a place of love. “He is doing the same thing by making [medecine bags] and giving them to people who need strength. I guess this is how he appreciates his life, being spiritual and recovering himself. He powerfully inspired me to be a nurse with heart.”
The Cultural Competence and Cultural Safety in Nursing Education framework manual published by the Aboriginal Nurses Association of Canada offers 6 core competencies to incorporate into nursing education curricula. At the top of the list is walking through the nursing journey with an understanding of the legacy of residential school and recognizing barriers to health equity that continue to impact First Nations, Metis and Inuit communities. One of those barriers is the absence of Indigenous perspective in health care.
“Elder Don showed people there is a different way to think about things. Like how he only uses traditional medicine. How he gets his strength and mental health through traditional practices… the medicine wheel encompasses well being- something that I think nursing is trying to do but hasn’t [accomplished] yet,” one student thoughtfully contributed.
Moving forward with nursing education necessitates sharing the truth of residential schools in order to develop a culturally safe practice. Do not wait for a challenging situation to learn this truth. We know that students retain the most information by hearing, seeing and doing. Incorporating opportunities outside of readings is integral to equipping nursing students with a holistic, critical and relational practice. Using traditional practices embedded with First Nations teachings, Elder Don reaches out to struggling individuals on the DTES and the greater Vancouver Area. Nurses are also in the position to help this population. For student nurses it can feel overwhelming to know where to begin. Here are some strategies student nurses can use, beginning now.
Learn about the territory you are in and acknowledge the community that existed pre-colonization. Normalize acknowledging territories during formal meetings and presentations to reduce feelings of discomfort that can arise. Be curious and ask questions with an open heart and genuine compassion, only after you have listened and observed. Seek out resources, partnerships and get involved! Lastly and perhaps most importantly, it is about treating each patient contextually to this particular place and time. In the clinical setting weighted by systemic structures, long hours, and staffing shortages, it can be easy and reactionary to hastily profile a patient or client. Kait pointedly summarizes how to address this reaction:
“Something that Elder Don said during his presentation has stuck with me. He said that he will never judge someone who is on the street because you never know what got them there, and what they may have overcome being there. That is something that I will carry with me.”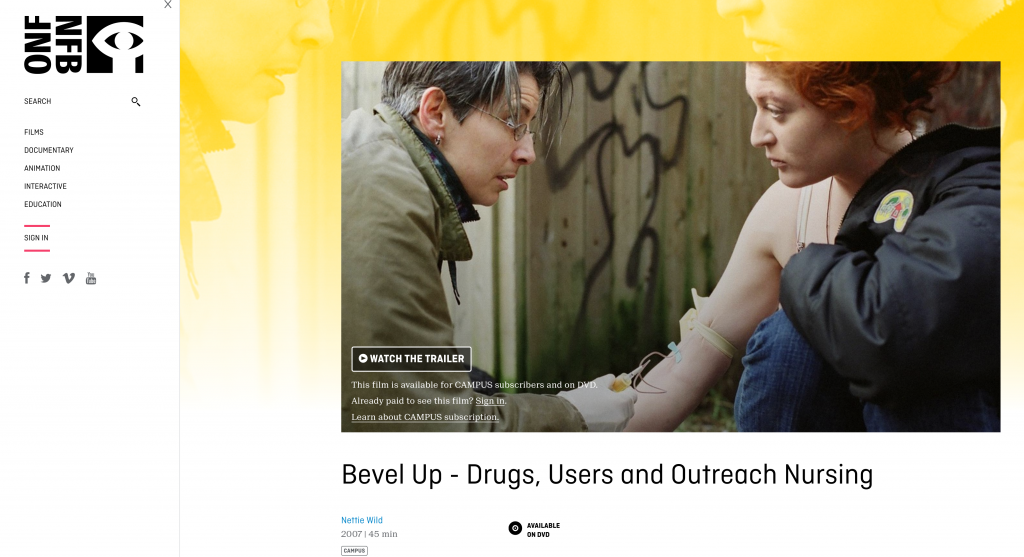

 Follow
Follow