Strokes are the fifth leading cause of deaths in North America. If one is fortunate enough to survive a stroke, the rehabilitation process is long and painful depending on the amount of damage done to the brain. There are two types of strokes – ischemic and hemorrhagic. Ischemic strokes are the result of a clot forming in an artery and preventing blood flow, whereas hemorrhagic strokes are the result of an artery bursting and and the brain literally bleeding out.
Many researchers have worked towards improving and developing treatments to reduce the amount of brain damage a patient suffers during a stroke. One of the events that takes place during a stroke is called excitotoxicity, where brain cells literally excite themselves to death.
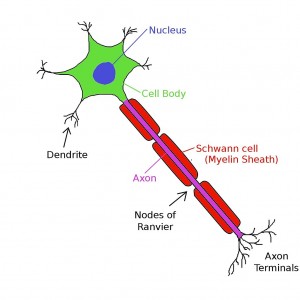
Receptors like NMDA as well as calcium are key culprits in causing damage to brain tissue. NMDA is a protein that is present on nerve cells and binds to the neurotransmitter glutamate. When a stroke occurs, nerve cells release large amounts of glutamate which bind to these NMDA receptors. The binding of glutamate to an NMDA receptor causes it to open. Calcium which is present in excess on the outside of the nerve cell, enters the cell. The calcium alongside with glutamate go on to wreck havoc in the nerve cell ultimately leading to its death.
Courtesy of Khashayar.
Dr. Nicolas Weilinger investigated what happens at a cellular level during a stroke and the mechanism which works to damage brain cells. While researching, Dr. Weilinger discovered a new signalling pathway that had broad reaching implications for brain physiology and pathology.
The findings of this study are important because current treatments in place to protect the brain during and after a stroke are not as effective as they should be. One of the main findings of Dr. Weilinger’s paper was that another channel much bigger than NMDA called pannexin gets activated during a stroke. Pannexin is physically connected to the NMDA receptor so when the NMDA receptor opens it signals pannexin to open as well. The opening of another channel therefore allows more calcium and glutamate to enter at an even faster pace. Using this information, a new drug was designed that would prevent the NMDA receptor from communicating with pannexin – in other words it would block the physical connection between the two proteins.
The wider implications of Weilinger’s paper is to hopefully improve stroke treatment. Future research into Dr. Weilinger’s findings could potentially be the first step in discovering a new drug type that can be used to reduce brain damage suffered during a stroke.
**We would like to thank Dr. Nicholas Weillinger for his time and the SCIE 300 team for guiding us and providing feedback.**
Harnoor, Khashayar, Matthew.