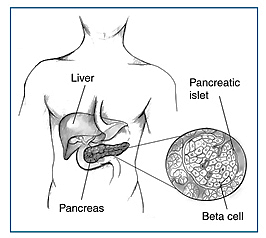
Type I diabetes is a condition characterized by destruction of pancreatic β-cells due to cell-mediated autoimmune attack. Insulin is not produced as result. Insulin enables cells to take up glucose from blood and use it for energy. It effects about 6% of the adult population worldwide. It accounts for 5-10% of all cases of diabetes. It is believed that the disease is caused by self-activation of white blood cells (responsible for body’s immunity) and instead of attacking foreign particles, they attack body organs and destroy their cells. T-lymphocytes (a type of white blood cell) attacks pancreatic β-cells by recognizing the islet auto-antigens. Auto-antigens are produced in body and immune system produces antibodies against it. As a result, body’s immune system turns against organs in body and starts destroying them.
At the time of diagnosis, almost all of cells are destroyed and the pancreas has lost the ability to produce insulin. This leads to patients using “exogenous” insulin or β-cells replacement, also called Islet cell transplantation. Type I diabetes has been categorized into two subtypes, Type 1A and type 2A. For patients diagnosed with type 1A the pathogenicity of the disease is due to autoimmune factors, whereas for type 2A, which is less frequent, our knowledge is very limited.

There are three million Canadians living with either type I or type II diabetes. Canada being one of the leading countries in the research of diabetes helps to improve the livelihood of Canadians diagnosed with type I diabetes. A group of Canadian researches in Edmonton have performed the first transplant using a new method. They were successful, so they published their results the year after, in the New England Journal of Medicine. Islet transplantation is an important method to treat type I diabetes. The Canadian Diabetes Association have spent five million dollars in research on type I diabetes and islet transplantation.
Islet cell transplantation is the only method to this day that re-establishes the endogenous insulin secretion in patients diagnosed with type I diabetes. There are two types of islet transplantation:
- Auto-transplantation
- Allo-transplantation
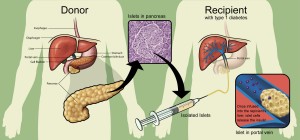
Auto-transplantation is performed following pancreatectomy (complete removal of the pancreas). The pancreas is removed in a hospital setting with the help of general anesthesia. The removed pancreas is extracted and purified. Finally, the islet cells are infused using a catheter into the patient’s liver. Interestingly, patients with type I diabetes cannot receive this treatment. Type I diabetics patients can not receive this treatment because their β-cells are destroyed as a result of autoimmune attack. Thus, removing their pancreas and purifying the cells is useless. This treatment is used for patients diagnosed with chronic pancreatitis (inflammation of pancreas).
The second method is still an experimental procedure. In this procedure islet cells from the pancreas of a deceased person are purified and injected into another person. It is often required to transplant two or more pancreases in order to stop the need for the insulin.
In conclusion, islet transplantation should be viewed as a method to decrease the onset of hypoglycemic episodes and improve glycemic control. Though, limitations of this procedure indicate that this procedure is not suitable for all type I diabetic patients.