Components of the Circulatory System: Part 1 – Blood
Blood is more than just a liquid it is a complex tissue that:
- Helps fights infection
- Regulates body temperature
- Transports nutrients, O2, metabolic wastes.
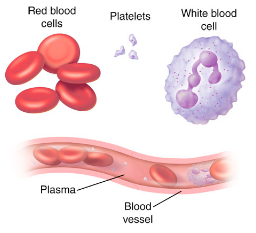
Made up of three kinds of cells transported in extracellular fluid called plasma.
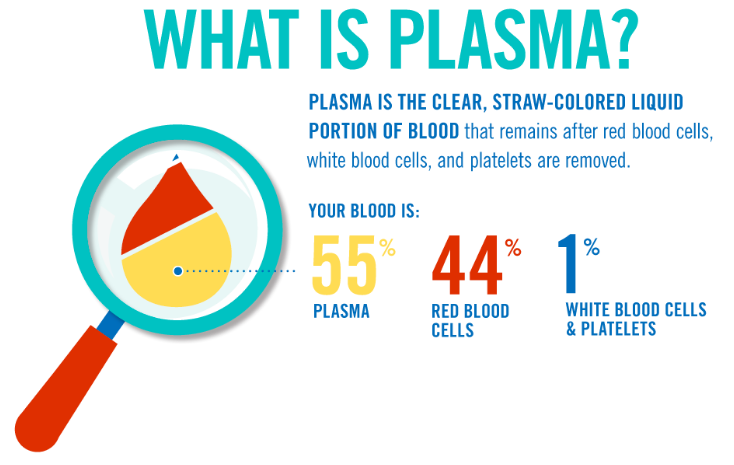
Approximately 55% of the blood plasma the remaining 45% is composed of blood cells
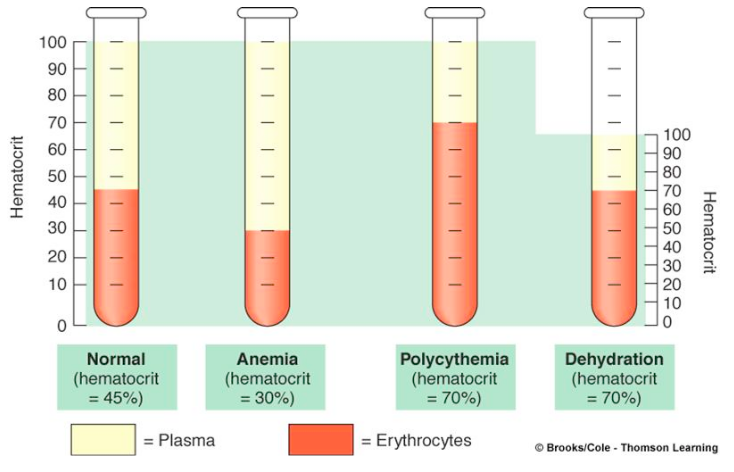
If blood is allowed to sit in a test tube without clotting, it will divide into two main parts: plasma and formed elements (blood cells)
Hematocrit – Ratio of red blood cells to total volume of blood (normal = 45% RBC)
Plasma
Plasma is ~90% water. Ions, nutrients, waste, and proteins are also present. Two groups of plasma proteins to know:
- Globulins (proteins made by the liver) help with antibody defense
- Fibrinogens are important in blood clotting (converted by platelets to fibrin during injury which closes damaged blood vessels)
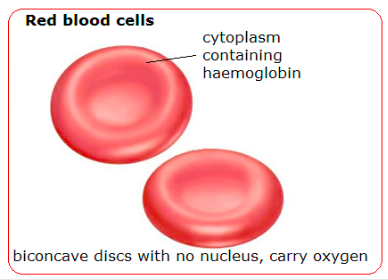
Red Blood Cells (Erythrocytes)
Red blood Cells (Erythrocytes) are continuously made in the bone marrow.
Structure:
- Biconcave disk with no nucleus
- Have “markers” called antigens on surface.
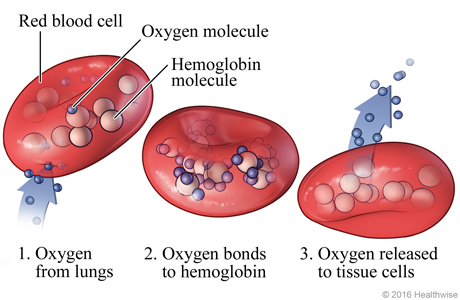
- Unique protein (hemoglobin) in cytoplasm
Function:
- Primary function of erythrocytes is the transport of oxygen.
- The presence of hemoglobin in RBCs increases the ability of the blood to carry oxygen by a factor of almost 70.
- Without a nucleus, RBCs cannot perform many cell functions therefore they have a short (120 day) life span
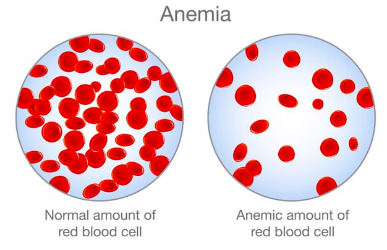
Now that we know the function of erythrocytes, What issues could arise from a lowered hematocrit?
Anemia is a condition where blood lacks healthy erythrocytes or hemoglobin
- This leads to a lack of oxygen being transported around the body.
- 5.6% of North Americans suffer from one of the 400 types of anemia.
The most common type is iron-deficiency anemia (iron is needed to produce hemoglobin)
Symptoms:
- Chest pain, fast heartbeat or shortness of breath
- Headache, dizziness or lightheadedness
- Extreme fatigue
- Weakness
- Pale skin
- Cold hands and feet
White Blood Cells – Leukocytes
White blood cells (Leukocytes) are made in the bone marrow (like all blood cells). Larger and less numerous than RBCs.
Structure:
- Many distinct types. All have a nucleus (making them easy to identify compared to RBCs)
- The shape and size of the nucleus, along with the granules in the cytoplasm are used to identify different leukocytes.
We can break white blood cells into two basic groups based on the presence of granule (visible small particles in the cytoplasm – ex. secretory vesicles) These groups are granulocytes and agranulocytes.
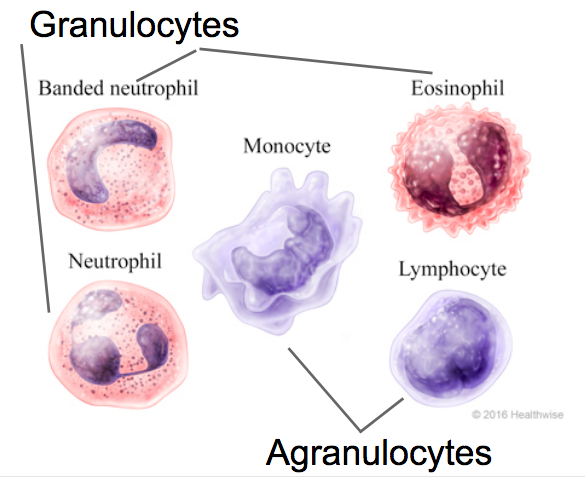
Granulocytes – Contains granules (small particles) in the cytoplasm – usually secretory vesicles or components that can lead to helpful immune responses (i.e. the Natural Killer Granulocyte contains components that lead to lysis of target cells)
- Usually multi-lobed nucleus
- ex. Neutrophil (the most common white blood cell), Eosinophil, Basophil.
Agranulocytes – No conspicuous granules in cytoplasm. Have specific roles in the immune response.
- Single nucleus
- ex. Monocytes (macrophages when in tissue) and lymphocytes
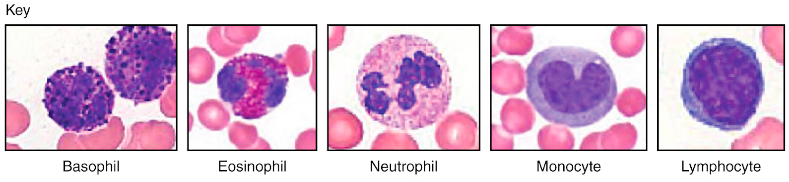
Figure 9: White blood cell identification
Two types of leukocytes to know (both are agranulocytes):
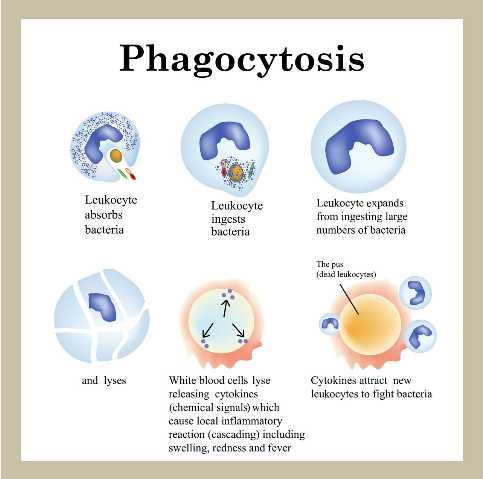
- Monocytes (macrophage) fight off bacteria, viruses and fungi.
- Monocytes are the biggest type of leukocyte
- Monocytes “eat” foreign particles through phagocytosis
Phagocytosis:
Once the microbe has been engulfed, the leukocyte releases enzymes that digest the microbe and the leukocyte itself.
Fragments of remaining from the white blood cell and invader are called pus.
- Lymphocytes produce antibodies in response to invading pathogens.
- Antibodies are very specific proteins that attach to invading pathogens.
- Antibodies bind to pathogens and cause them to agglutinate (clump together)
Platelets
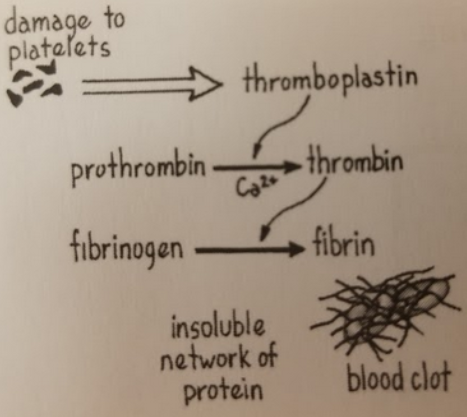
Platelets (thrombocytes) are small, fragile cell fragments involved with the blood clotting response.
Structure:
- No nucleus.
- Smallest of the blood cells
- Shaped like a “plate”
- Contain the enzyme thromboplastin – which catalyzes the reaction of the protein prothrombin to thrombin (needs Ca2+)

Formation of Blood Clots
- Circulating platelets rub against a rough edge of damaged blood vessel and release thromboplastin.
- Thromboplastin catalyzes the conversion from prothrombin into thrombin (needs Ca2+)
- Thrombin converts fibrinogen (glycoprotein) into fibrin.
- Fibrin is insoluble – this causes it to trap blood cells and create a clot.
Blood Cell Summary
- Plasma is the extracellular fluid which blood cells, proteins, nutrients, waste circulate in (90% water)
- Three types of blood cells (formed elements – 45% of blood):
- Erythrocytes – No Nucleus, biconcave disk. Carries oxygen.
- Leukocytes – Nucleus, amoebic (irregular shape) Immune response.
- Thrombocytes – Cell fragments. Blood clotting.
- Erythrocytes – No Nucleus, biconcave disk. Carries oxygen.
- Lower RBC/hemoglobin count = Anemia which leads to fatigue (Affects 5.6% of North Americans)
- Sickle-Cell anemia is a genetic disorder that causes sickle-shaped RBCs that struggle to transport oxygen (From lab)
In more depth:
Blood Types
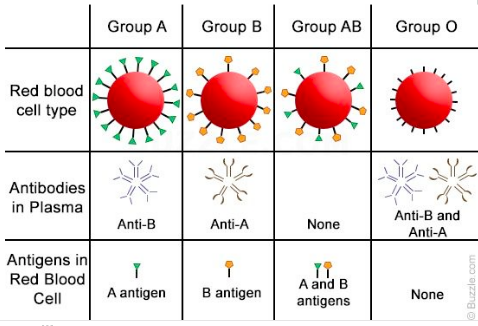
Human blood is classified according to the antigens present on the surface of the red blood cells.
Antigens are proteins found on blood cells/pathogens capable of stimulating an immune response.
Most common = ABO grouping.
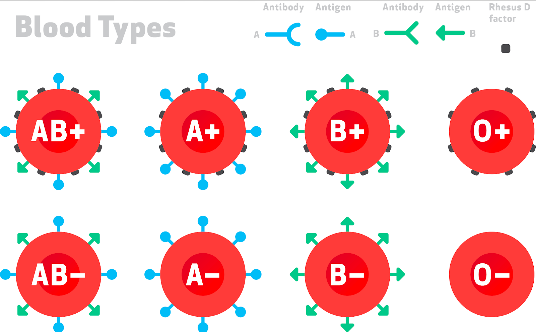
If blood cells have A antigens on the surface = Blood type A
Antigen B = Blood Type B
Antigen A and B = Blood Type AB
Neither antigen = Blood Type O
Antibodies and blood
Lymphocytes produce antibodies that are NOT found on the body’s blood cells.
Ex. If you are blood type A (cells have A antigens) lymphocytes will create antibody B.
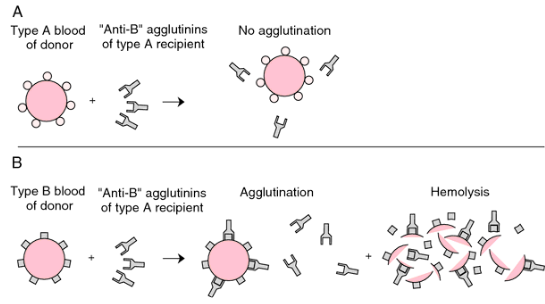
If an antibody matches and binds to a cell/pathogen – agglutination occurs leading to blocked capillaries.
To summarize:
- Humans blood group is based on what antigens are on the cell surface – A, B, BOTH, OR NEITHER.
- Antibodies are produced by lymphocytes that do not match/bind to the body’s own antigens.
- Pathogens/invaders get bound by antibodies causing them to clump (agglutinate)
Antigens/ Antibodies act as a lock and key mechanism leading to an immune response!
Can we receive a blood transfusion from anyone?
No. If a person is given blood that is different from their own the persons antibodies could match and bind to the new blood causing agglutination – just like what would happen with a foreign bacteria.
One last note:
Rh (Rhesus Factor) – another antigen occurring on the red blood cells of many humans (around 85 percent). Humans can be Rh + OR Rh – (No antigen).
Rh – = Rh antibodies in plasma – cannot accept from Rh+ people.
This brings up the total blood types in humans to 8.
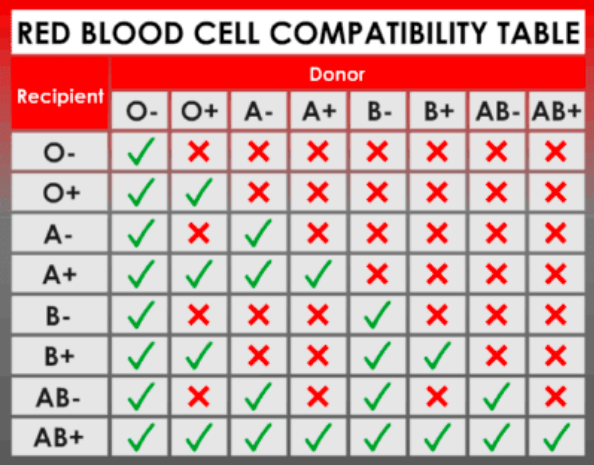
O- Blood is a universal donor. It can go to anyone since the blood cells have no antigens! This means there is no binding sites for antibodies.
AB+ Blood is a universal recipient. Any blood can be given since they have no antibodies for blood groups in their plasma/do not produce antibodies for A/B/RH. No antibodies = no binding = no immune response to the blood.
Blood typing game! Get some practice here!
Genetics: A Crash Course
Genetics crash course PDF of notes
Review Questions:
- Compare and contrast closed and open circulatory systems.
- What problems could arise from a lowered hematocrit?
- Could DNA replication take place in erythrocytes? Why or why not? What about leukocytes? Platelets?
- What causes the production of pus?
- How does clotting occur in blood? Include the role of platelets and the flowchart of steps leading to fibrin conversion.
- Explain why type O blood is considered to be the universal donor. Why is type AB considered to be the universal recipient?
- Define antigen and antibody.
- How does Rh-positive blood differ from Rh-negative blood?
- What is the breakdown of blood volume? (I.e. Plasma is the largest at 55% of blood)
- What antigens are on the surface of erythrocytes of a person with B+ blood? What antibodies do they produce?
- A mother has AB blood and her husband has A blood. There child has B type blood. Is this possible? Use punnet squares to help you explain your answer.
Comments by shaun pletsch