3. Regulation of Breathing
Carbon Dioxide and Hydrogen Ions (H+) in the blood control breathing rate.
- CO2 will build up in the blood due to cellular respiration, increasing the concentration to a threshold level.
- Chemoreceptors in the aorta and carotid arteries detect this and signal the breathing centre in the medulla oblongata.
- The medulla oblongata begin signaling an inhalation response – causing the diaphragm and intercostal muscles to contract. (increasing volume, and creating negative pressure – as learned earlier).
- Air flows into alveoli, and the alveolar walls expand and stretch
- Stretch Receptors in the alveoli walls detect this stretching and signal the medulla oblongata to stop contraction of diaphragm/intercostal muscles.
So breathing rate is controlled by the autonomic nervous system (unconscious functions such as heart rate, digestive processes, breathing).
However, breathing rate is also subject to partial conscious control.Why do you think that is?
Benefits:
- Hide from predators/ quiet
- Speech
- Ability to dive/enter water
Mammalian Diving Reflex:
- Physiological reflexes that favor oxygen to heart/brain
- Signals by holding breath, submersion in cold H20, and wetness in the nostrils
- Originates and signals from the same chemoreceptors in the carotid arteries.
- Leads to:
- 1) Bradycardia
- 2) Vasoconstriction (especially in arms/legs – leading to smaller circuit)
- Leads to:
4. Gas Exchange
Please note: All equations related to gas exchange are not present in these notes. Instead, you will have to build the equations using these notes and looking at diagrams provided during our Gas Exchange: Building Equations group assignment.
Recall:
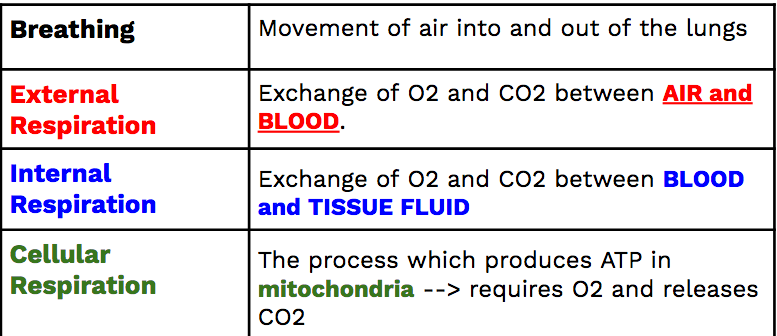
External Respiration
Basics:
- There is diffusion of oxygen into the pulmonary capillaries and the diffusion of CO2 (+ some H20) into the alveoli to be exhaled.
- Gas exchange occurs through diffusion alone – remember diffusion is movement from high concentration to low concentration:
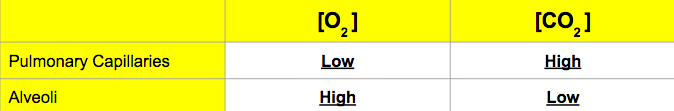
Think: How is diffusion of gas in the alveoli and capillaries possible?
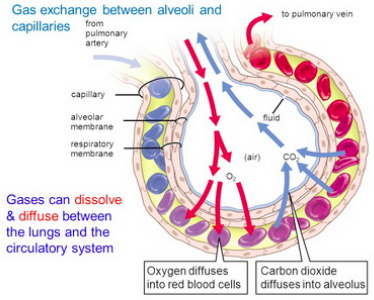
In Alveoli:
- Blood at alveoli ~37°C and a pH of ~7.38.
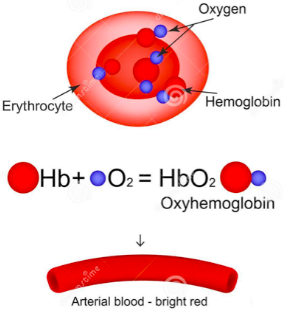
- Conditions cause oxygen to bind with the available hemoglobin in the blood.
- This creates oxyhemoglobin – HbO2
- As you learned, this improves blood’s ability to carry oxygen by 70 times.
Internal Respiration
In the tissues:
- Temperature in tissue capillaries is ~38°C and a pH of ~7.35 (warmer/more acidic than alveoli)
- Conditions cause hemoglobin to release oxygen.
- Oxyhemoglobin (HbO2) returns to hemoglobin (Hb) and and Oxygen (O2)
- Fluids/oxygen/nutrients enter tissues (remember last unit?)
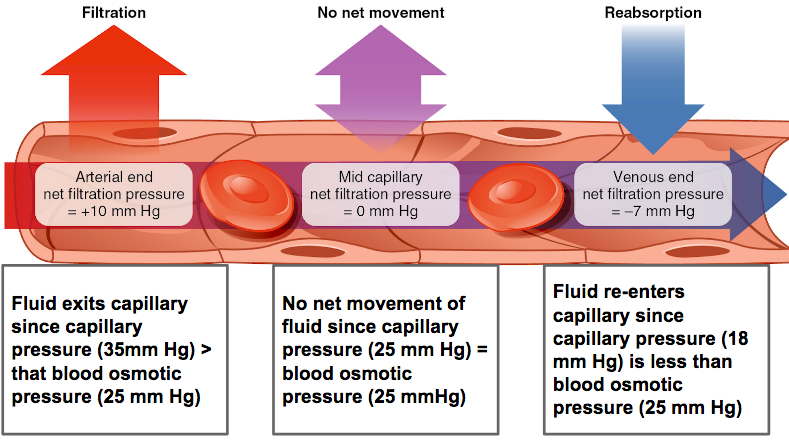
- On the venule side of the tissue capillaries, a higher osmotic pressure pushes water/CO2 and waste back into the capillaries.
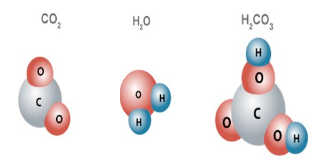
- The CO2 reacts with H20 to create carbonic acid (H2CO3 )
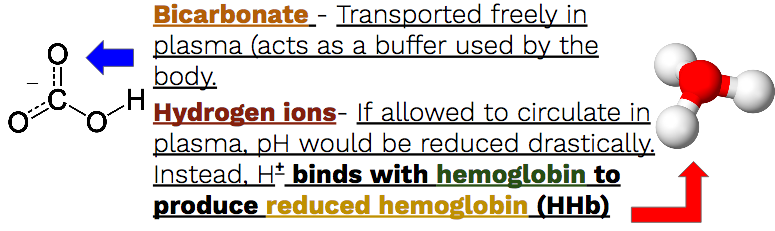
- Carbonic acid (H2CO3 ) -> Quickly dissociates into Bicarbonate ions (HCO3– ) and hydrogen ions (H+ ), catalyzed by carbonic anhydrate.
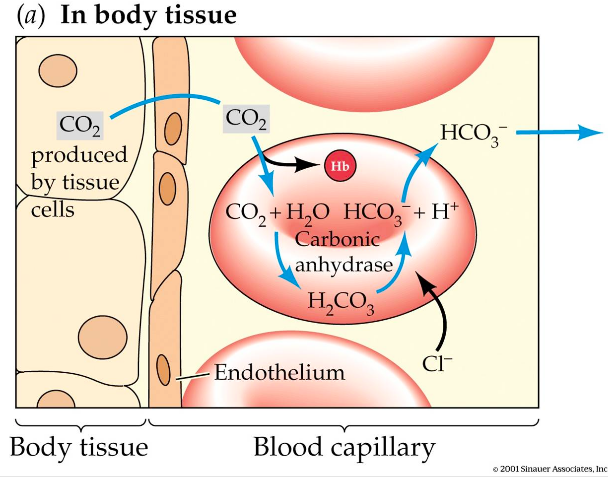
But, does all CO2 bind with H20?
- Some CO2 binds with hemoglobin to create carbaminohemoglobin (HbCO2)
- Some CO2 dissolves in the blood plasma
Return to alveoli:
- Blood returning the alveoli has:
-
- Transporting bicarbonate (HCO3-) ions
- Transporting some dissolved CO2
- Hemoglobin is transporting H+ (Reduced hemoglobin – HHb)
- OR hemoglobin is transporting CO2 (carbaminohemoglobin –HbCO2)
-
- In the alveoli temperature is lower and pH is higher (~37°C / pH of ~7.38)
- Hemoglobin releases H+ and CO2
- Carbonic anhydrase (the enzyme that catalyzed the reaction before) catalyzes the reverse reaction from bicarbonate and hydrogen to carbonic acid.
- Carbonic acid is catalyzed back into CO2 and H20.
Summary:
- Oxygen moves into the alveolar capillaries due to diffusion – it binds with hemoglobin on RBCs for transport.
- Once at tissue capillaries, the change in conditions cause hemoglobin to release oxygen which crosses into the tissues.
- CO2 enters the capillaries at the venule side and can either: 1) Bind with H20 to produce carbonic acid, 2) Dissolve in the plasma, 3) Bind to hemoglobin to produce carbaminohemoglobin.
- The carbonic acid created quickly breaks down into bicarbonate ions and hydrogen ions.
- Back at the alveoli, the conditions change again, causing hemoglobin to release hydrogen ions and CO2. Carbonic anhydrase catalyzes the reverse reaction from bicarbonate and hydrogen into carbonic acid and then into CO2 and water.
- CO2 and water diffusion out into the alveoli and are exhaled.
All information regarding tidal volume and vital capacity are in the background information provided in our lab Measuring Lung Capacity.
Comments by shaun pletsch