Please take notes on urine formation as homework (May 14th). You will be allowed to use these notes and the urinary structure notes to complete an in-class “quiz” May 16th. No notes/homework done means you cannot bring these in. I will print a companion diagram sheet for you and give it to you on May 16th.
Note: this video goes deeper than needed and into the final set of our notes – hormones and regulation!
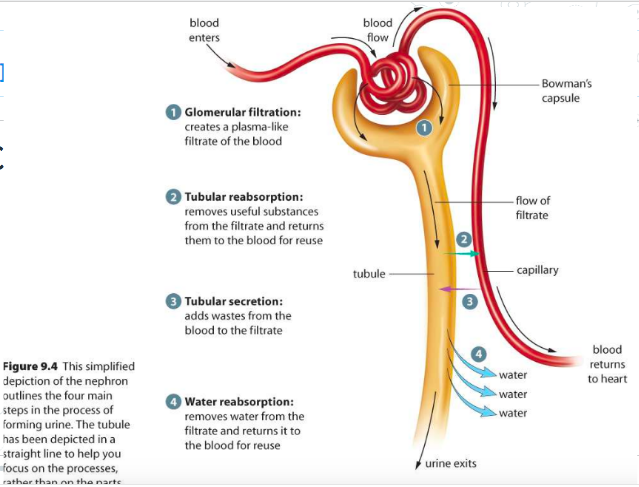
Formation of Urine
Three stages of urine formation:
- Filtration – Removing maximum waste from blood into nephron and creating a filtrate.
- Reabsorption – Bringing useful molecules back into the blood
- Secretion (aka tubular excretion) – Bringing as much harmful molecules from the blood as possible.
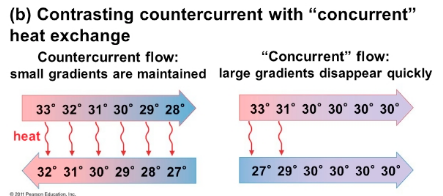
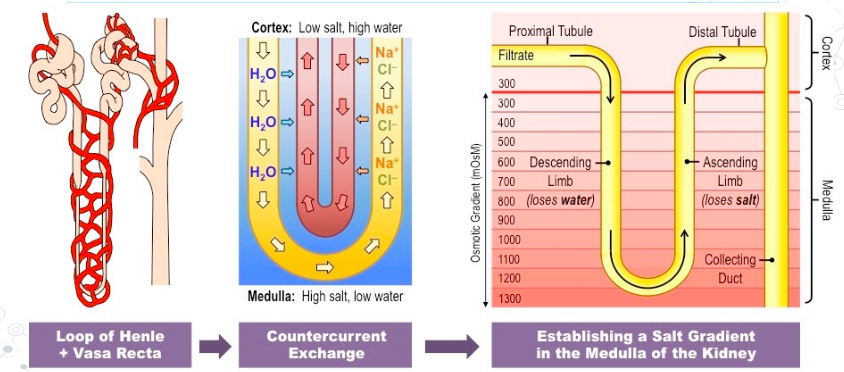
There is a countercurrent exchange occurring between the nephron and the peritubular capillary network.
- This allows for osmotic gradients to be maintained throughout the formation process.
- More Efficient
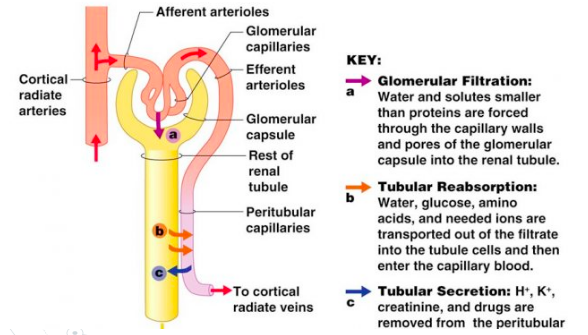
1. Filtration
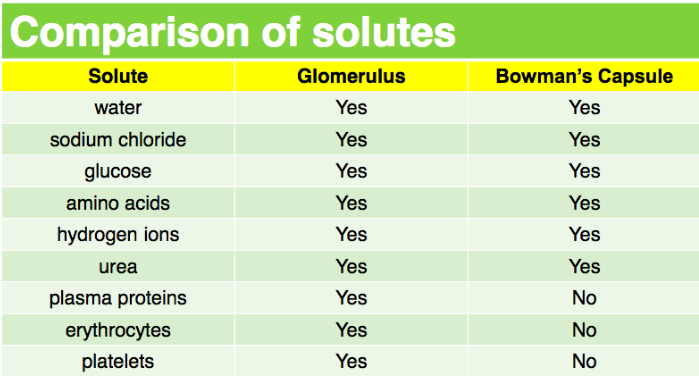
At the glomerulus there is very high pressure, thus this type of filtration is called pressure filtration.
- The substances removed create a plasma-like filtrate in the Bowman’s capsule
Things that are filtered into the Bowman’s capsule from the blood:
- Water
- NaCl
- Glucose
- H+
- Urea/Uric acid
Things that are not filtered into the Bowman’s capsule from the blood:
- Plasma proteins (too big)
- Blood cells (too big)
- Some water, salts, glucose, amino acids, and H+ stay
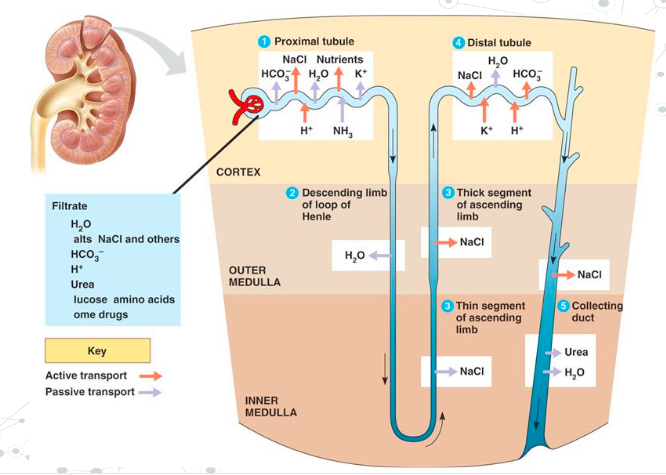
2. Reabsorption
Occurs at the proximal convoluted tubule and the Loop of Henle.
In the proximal convoluted tubule:
- Selective reabsorption: Nephron actively transports glucose, amino acids, and Na+ ions back into the blood (useful molecules – takes ATP).
- Negative ions (i.e. Cl-) follow the positive ion (Na+) passively
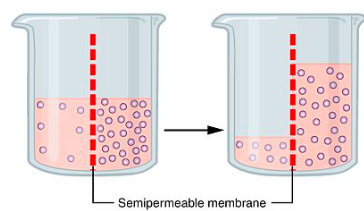
More ions/molecules moving back into the blood concentrates the blood making an osmotic gradient (Difference in concentration between two solutions )
- This causes water to reenter the blood vis osmosis.
- This causes the filtrate to become concentrated as it moves through the proximal convoluted tubule.
In the Loop of Henle:
- In the descending loop: not permeable to ions, permeable to water.
- Water leaves nephron, urine becomes more concentrated
- In the ascending loop: permeable to ions, not permeable to water.
- Na+ leaves the nephron, fluid around descending loop becomes concentrated
- This allows for more water reabsorption (back into the blood) anytime the nephron passes back into that region (even the collecting duct!)
3. Secretion
Occurs in the distal convoluted tubule (+ little in collecting duct).
- Movement of waste still in blood into nephron
- Active Transport: Urea, Uric acid, excess K+, vitamin C, drugs, H+.
- Some water enters the urine again
- The urine is now collected in the collecting ducts and carried to the bladder through the ureter for excretion.
Summary:
- Urine is formed through a modified capillary fluid exchange between the blood and the nephron.
- Filtration: Filtrate enters the nephron from the Glomerulus (very high pressure).
- Filtration: Water, NaCl, Glucose, H+, Urea/Uric acid, enter nephron.
- Reabsorption – Proximal Tubule: Selective reabsorption of glucose, amino acids, and Na+ (this is active transport – takes energy) Cl- passively follows.
- Reabsorption – Loop of Henle: Descending loop – water leaves nephron (osmosis), enters blood.
- Reabsorption – Loop of Henle: Ascending loop – Na+ leaves nephron enters blood (lower, thin section – Na leaves passively, higher, thick section – Na+ leaves with active transport.
- Secretion (Tubular excretion): Occurs in distal convoluted tubule. Active Transport of Urea, Uric acid, excess K+, vitamin C, drugs, H+ back into the nephron.
Comments by shaun pletsch